Male Pelvis: Difference between revisions
Jump to navigation
Jump to search
Urology4all (talk | contribs) No edit summary |
Urology4all (talk | contribs) |
||
| (7 intermediate revisions by the same user not shown) | |||
| Line 14: | Line 14: | ||
* Cooper (pectineal) ligament | * Cooper (pectineal) ligament | ||
** Overlies the pectineal line and offers a sure hold for sutures in hernia repairs and urethral suspension procedures | ** Overlies the pectineal line and offers a sure hold for sutures in hernia repairs and urethral suspension procedures | ||
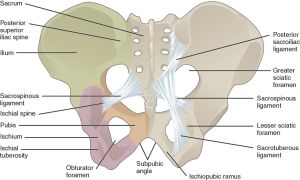
[[File:817 Ligaments of Pelvis.jpg|thumb|[[commons:File:817_Ligaments_of_Pelvis.jpg|Source]]]] | |||
== Soft tissues of the pelvis == | == Soft tissues of the pelvis == | ||
| Line 84: | Line 84: | ||
* '''Source: branch of the common iliac artery''' | * '''Source: branch of the common iliac artery''' | ||
* '''Location: Follows the medial border of the iliopsoas muscle''' along the arcuate line '''and leaves the pelvis beneath the inguinal ligament and continues as the femoral artery''' | * '''Location: Follows the medial border of the iliopsoas muscle''' along the arcuate line '''<span style="color:#ff0000">and leaves the pelvis beneath the inguinal ligament and continues as the femoral artery''' | ||
* '''Surgical considerations''' | * '''Surgical considerations''' | ||
** '''Only vessel in the pelvis without adequate collateral circulation; if ligated will cause significant sequella''' | ** '''Only vessel in the pelvis without adequate collateral circulation; if ligated will cause significant sequella''' | ||
* '''Branch (1):''' | * '''<span style="color:#ff0000">Branch (1):''' | ||
** '''Inferior epigastric artery'''§ | ** '''<span style="color:#ff0000">Inferior epigastric artery'''§ | ||
*** '''Source: branch of the external iliac artery''' | *** '''Source: branch of the external iliac artery''' | ||
*** '''Location''' | *** '''Location''' | ||
| Line 98: | Line 98: | ||
**** '''Inferior: inguinal ligament''' | **** '''Inferior: inguinal ligament''' | ||
*** Pierces transversalis fascia as it continues to ascend superiorly and superficially, until it levels posterior to rectus once is crosses the arcuate line/linea semicircularis. Continues to rise superiorly until it terminates by piercing rectus abdominis and branches and forms and anastamosis with the superior epigastric arteries, at approximately the level of the superior epigastric arteries. | *** Pierces transversalis fascia as it continues to ascend superiorly and superficially, until it levels posterior to rectus once is crosses the arcuate line/linea semicircularis. Continues to rise superiorly until it terminates by piercing rectus abdominis and branches and forms and anastamosis with the superior epigastric arteries, at approximately the level of the superior epigastric arteries. | ||
** '''Branches (3):''' | *** '''<span style="color:#ff0000">Branches (3):''' | ||
**# '''Deep circumflex iliac – supplies inguinal ligament and surrounding structures laterally (See Figure)''' | ***# '''<span style="color:#ff0000">Deep circumflex iliac</span> – supplies inguinal ligament and surrounding structures laterally (See Figure), can also arise directly from external iliac''' | ||
**# '''Pubic''' – supplies inguinal ligament and surrounding structures medially | ***# '''<span style="color:#ff0000">Pubic</span>''' – supplies inguinal ligament and surrounding structures medially | ||
**# '''Cremesteric – supplies vas deferens and testis''' | ***# '''<span style="color:#ff0000">Cremesteric</span> – supplies vas deferens and testis''' | ||
**## '''In 25% of people, an accessory obturator artery arises from the inferior epigastric artery''' and runs medial to the femoral vein to reach the obturator canal. This vessel must be avoided during obturator lymph node dissection | ***## '''In 25% of people, an accessory obturator artery arises from the inferior epigastric artery''' and runs medial to the femoral vein to reach the obturator canal. This vessel must be avoided during obturator lymph node dissection | ||
**## '''Rectus muscle and overlying skin''' | ***## '''Rectus muscle and overlying skin''' | ||
** '''Surgical considerations''' | ** '''Surgical considerations''' | ||
*** '''Can be ligated without complication because the rectus is richly collateralized''' from above and laterally | *** '''Can be ligated without complication because the rectus is richly collateralized''' from above and laterally | ||
| Line 112: | Line 112: | ||
* '''Source: common iliac artery''' | * '''Source: common iliac artery''' | ||
* '''Location: Descends in front of the SI joint''' | * '''Location: Descends in front of the SI joint''' | ||
* '''Branches (2): divides into an anterior and a posterior trunk''' approximately 3-4 cm from the bifurcation. | * '''<span style="color:#ff0000">Branches (2): divides into an anterior and a posterior trunk''' approximately 3-4 cm from the bifurcation. | ||
** '''Posterior trunk''' | ** '''<span style="color:#ff0000">Posterior trunk''' | ||
*** '''Surgical considerations''' | *** '''Surgical considerations''' | ||
**** '''Rarely seen during pelvic surgery''' | **** '''Rarely seen during pelvic surgery''' | ||
*** '''Branches (3) S-GALLS''' | *** '''<span style="color:#ff0000">Branches (3) S-GALLS''' | ||
***# '''Superior Gluteal''' | ***# '''<span style="color:#ff0000">Superior Gluteal''' | ||
***#* '''Exits the greater sciatic foramen''' | ***#* '''Exits the greater sciatic foramen''' | ||
***#* Supplies gluteus muscles and overlying skin | ***#* Supplies gluteus muscles and overlying skin | ||
***# '''Ascending Lumbar'''/iliolumbar | ***# '''<span style="color:#ff0000">Ascending Lumbar'''/iliolumbar | ||
***#* Supplies the posterior abdominal wall (psoas and quadratus lumborum muscles and adjacent structures) | ***#* Supplies the posterior abdominal wall (psoas and quadratus lumborum muscles and adjacent structures) | ||
***# '''Lateral Sacral''' | ***# '''<span style="color:#ff0000">Lateral Sacral''' | ||
***#* Passes medially to join the middle sacral branches from the aorta at the sciatic foramina | ***#* Passes medially to join the middle sacral branches from the aorta at the sciatic foramina | ||
***#* Supplies sacral nerves and sacrum | ***#* Supplies sacral nerves and sacrum | ||
** '''Anterior trunk''' | ** '''<span style="color:#ff0000">Anterior trunk''' | ||
*** '''Surgical considerations''' | *** '''Surgical considerations''' | ||
**** '''The primary branches identified during retroperitoneal surgery include the superior vesical artery, the uterine artery, and occasionally the obturator artery.''' | **** '''The primary branches identified during retroperitoneal surgery include the superior vesical artery, the uterine artery, and occasionally the obturator artery.''' | ||
*** '''Branches (6) Mr. U IPIG SVIVO''' | *** '''<span style="color:#ff0000">Branches (6) Mr. U IPIG SVIVO''' | ||
***# '''Umbilical''' | ***# '''<span style="color:#ff0000">Umbilical''' | ||
***#* In fetus, paired arteries surroud bladder and extend into umbilical cord. | ***#* In fetus, paired arteries surroud bladder and extend into umbilical cord. | ||
***#* '''After birth, a portion regresses to become the medial umbilical ligaments, while a portion remains open as the''' '''first branch off of the anterior trunk''' | ***#* '''After birth, a portion regresses to become the medial umbilical ligaments, while a portion remains open as the''' '''first branch off of the anterior trunk''' | ||
| Line 145: | Line 145: | ||
***#***** Can also come off the umbilical artery or the inferior vesical artery. | ***#***** Can also come off the umbilical artery or the inferior vesical artery. | ||
***#***** Travels the length of the vas to meet the cremasteric and testicular arteries distally. Because of these anastomoses, the testicular artery may be sacrificed without compromising the viability of the testis. | ***#***** Travels the length of the vas to meet the cremasteric and testicular arteries distally. Because of these anastomoses, the testicular artery may be sacrificed without compromising the viability of the testis. | ||
***# '''Obturator''' | ***# '''<span style="color:#ff0000">Obturator''' | ||
***#* Variable in origin | ***#* Variable in origin | ||
***#* '''Travels through the obturator fossa''' '''medial and posterior to the obturator nerve''' | ***#* '''Travels through the obturator fossa''' '''medial and posterior to the obturator nerve''' | ||
***#* Supplies adductor muscles of the thigh and overlying skin | ***#* Supplies adductor muscles of the thigh and overlying skin | ||
***# '''Inferior Vesical''' | ***# '''<span style="color:#ff0000">Inferior Vesical''' | ||
***#* Supplies bladder base, seminal vesicle, prostate, lower ureter, and the neurovascular bundle | ***#* Supplies bladder base, seminal vesicle, prostate, lower ureter, and the neurovascular bundle | ||
***# '''Middle Rectal''' | ***# '''<span style="color:#ff0000">Middle Rectal''' | ||
***#* Gives small branches to the seminal vesicles and prostate and anastomoses with the inferior and superior rectal arteries in the rectal wall. | ***#* Gives small branches to the seminal vesicles and prostate and anastomoses with the inferior and superior rectal arteries in the rectal wall. | ||
***#* Supplies rectum, ureter, and bladder | ***#* Supplies rectum, ureter, and bladder | ||
***# '''Internal Pudendal''' | ***# '''<span style="color:#ff0000">Internal Pudendal''' | ||
***#* Terminal branch of the internal iliac artery | ***#* Terminal branch of the internal iliac artery | ||
***#* '''Location''' | ***#* '''Location''' | ||
***#** '''Leaves the pelvis through the greater sciatic foramen''', passes around the sacrospinous ligament, and enters the lesser sciatic foramen to gain access to the perineum. | ***#** '''Leaves the pelvis through the greater sciatic foramen''', passes around the sacrospinous ligament, and enters the lesser sciatic foramen to gain access to the perineum. | ||
***#** After entering the perineum through the lesser sciatic foramen, the artery runs in a fascial sheath on the '''medial aspect of obturator internus, which is the pudendal canal (of Alcock)'''. | ***#** After entering the perineum through the lesser sciatic foramen, the artery runs in a fascial sheath on the '''medial aspect of obturator internus, which is the pudendal canal (of Alcock)'''. | ||
***#* '''Branches (5): IPP BC''' | ***#* '''<span style="color:#ff0000">Branches (5): IPP BC''' | ||
***#*# '''Inferior rectal artery''' | ***#*# '''<span style="color:#ff0000">Inferior rectal artery''' | ||
***#*# '''Perineal artery''' | ***#*# '''<span style="color:#ff0000">Perineal artery''' | ||
***#*# '''Posterior scrotal/labial''' | ***#*# '''<span style="color:#ff0000">Posterior scrotal/labial''' | ||
***#*# '''Artery of Bulb of penis''' | ***#*# '''<span style="color:#ff0000">Artery of Bulb of penis''' | ||
***#*# '''Common penile artery (terminal branch)''' | ***#*# '''<span style="color:#ff0000">Common penile artery (terminal branch)''' | ||
***#*#* '''The common penile artery branches into the (3):''' | ***#*#* '''<span style="color:#ff0000">The common penile artery branches into the (3):''' | ||
***#*#*# '''Cavernosal artery''' | ***#*#*# '''<span style="color:#ff0000">Cavernosal artery''' | ||
***#*#*# '''Bulbourethral artery''' | ***#*#*# '''<span style="color:#ff0000">Bulbourethral artery''' | ||
***#*#*# '''Dorsal artery''' | ***#*#*# '''<span style="color:#ff0000">Dorsal artery''' | ||
***#* Supplies rectum, perineum, and external genitalia | ***#* Supplies rectum, perineum, and external genitalia | ||
***#* '''Note that the external pudendal artery comes from the femoral artery and the superior rectal artery comes from the inferior mesenteric artery''' | ***#* '''Note that the external pudendal artery comes from the femoral artery and the superior rectal artery comes from the inferior mesenteric artery''' | ||
***# '''Inferior Gluteal''' | ***# '''<span style="color:#ff0000">Inferior Gluteal''' | ||
***#* '''Travels through the greater sciatic foramen''' | ***#* '''Travels through the greater sciatic foramen''' | ||
***#* Supplies gluteus muscles and overlying skin | ***#* Supplies gluteus muscles and overlying skin | ||
***# '''Vaginal''' '''(if female)''' | ***# '''<span style="color:#ff0000">Vaginal''' '''(if female)''' | ||
***# '''Uterine (if female)''' | ***# '''<span style="color:#ff0000">Uterine (if female)''' | ||
***#* Often branches off of superior vesical artery | ***#* Often branches off of superior vesical artery | ||
***#* '''Passes anterior to ureter''' and enters the lateral uterus at the level of the internal cervical os to meet ovarian artery | ***#* '''Passes anterior to ureter''' and enters the lateral uterus at the level of the internal cervical os to meet ovarian artery | ||
| Line 202: | Line 202: | ||
'''Somatic nerves of the lower abdomen and pelvis''' | '''Somatic nerves of the lower abdomen and pelvis''' | ||
{| class="wikitable" | {| class="wikitable" | ||
|'''Nerve''' | |'''<span style="color:#ff0000">Nerve''' | ||
|'''Origin''' | |'''<span style="color:#ff0000">Origin''' | ||
|'''Motor''' | |'''<span style="color:#ff0000">Motor''' | ||
|'''Sensory''' | |'''<span style="color:#ff0000">Sensory''' | ||
|- | |- | ||
|Iliohypogastric | |Iliohypogastric | ||
| Line 212: | Line 212: | ||
|Lower anterior abdominal wall | |Lower anterior abdominal wall | ||
|- | |- | ||
|'''Ilioinguinal''' | |'''<span style="color:#ff0000">Ilioinguinal''' | ||
|'''L1''' | |'''<span style="color:#ff0000">L1''' | ||
| | | | ||
|'''Anterior scrotum''' (or mons pubis and labium majus)''', root of penis, and upper medial thigh''' | |'''<span style="color:#ff0000">Anterior scrotum</span>''' (or mons pubis and labium majus)''', root of penis, and upper medial thigh''' | ||
|- | |- | ||
|'''Genitofemoral''' | |'''<span style="color:#ff0000">Genitofemoral''' | ||
|'''L1, L2''' | |'''<span style="color:#ff0000">L1, L2''' | ||
|'''Genital branch: cremaster muscle''' | |'''<span style="color:#ff0000">Genital branch: cremaster muscle''' | ||
|'''Genital branch: anterior scrotum''' (or mons pubis and labium majus) | |'''<span style="color:#ff0000">Genital branch: anterior scrotum</span>''' (or mons pubis and labium majus) | ||
'''Femoral branch: upper anterior thigh''' | '''<span style="color:#ff0000">Femoral branch: upper anterior thigh''' | ||
|- | |- | ||
|'''Lateral femoral cutaneous nerve of thigh''' | |'''Lateral femoral cutaneous nerve of thigh''' | ||
| Line 229: | Line 229: | ||
|'''Sensory to anterior and lateral thigh''' | |'''Sensory to anterior and lateral thigh''' | ||
|- | |- | ||
|'''Femoral''' | |'''<span style="color:#ff0000">Femoral''' | ||
|'''L2, L3, L4''' | |'''<span style="color:#ff0000">L2, L3, L4''' | ||
|'''Extensors of the knee''' | |'''<span style="color:#ff0000">Extensors of the knee''' | ||
|'''Anterior thigh and medial leg''' | |'''<span style="color:#ff0000">Anterior thigh and medial leg''' | ||
|- | |- | ||
|'''Obturator''' | |'''<span style="color:#ff0000">Obturator''' | ||
|'''L2, L3, L4''' | |'''<span style="color:#ff0000">L2, L3, L4''' | ||
|'''ADDuctors of the thigh''' | |'''<span style="color:#ff0000">ADDuctors of the thigh''' | ||
|'''Medial thigh''' | |'''<span style="color:#ff0000">Medial thigh''' | ||
|- | |- | ||
|Lumbosacral trunk | |Lumbosacral trunk | ||
Latest revision as of 20:57, 16 March 2024
Bony pelvis[edit | edit source]
- The pelvic bones are the:
- Sacrum
- Termination of the axial skeleton
- 3 innominate bones:
- Ilium
- Ischium
- Pubis
- The ischium and pubis also meet below, in the center of the inferior ramus, to form the obturator foramen
- Sacrum
- Ischial spine
- A small posterior point between the ramus and the body of the ischium
- Cooper (pectineal) ligament
- Overlies the pectineal line and offers a sure hold for sutures in hernia repairs and urethral suspension procedures
Soft tissues of the pelvis[edit | edit source]
- Perineal body
- Fibrous membrane consisting of muscle and collagenous and elastic fibers
- Pyramid-shaped structure at the central point of the perineum
- Defines the urogenital diaphragm; represents the point of fusion between the free posterior edge of the urogenital diaphragm and the posterior apex of the urogenital hiatus
- Forms the hub of pelvic support. Virtually every pelvic muscle (superficial and deep transverse perinei, bulbospongiosus, levator ani, rectourethralis, external anal sphincter, striated urethral sphincter) and fascia (perineal membrane, Denonvilliers, Colles, and endopelvic) inserts into the perineal body
- Tendinous arch or the arcus tendinous
- Thickened band of pelvic fascia that runs from the ischial spine to the pubic bone
- Originates from the pubic bone laterally and is connected to the pubovesical ligament medially and the tendinous arch of the levator ani.
- Present in males and females
- Ligaments
- Inguinal ligament
- Superior attachment: anterior superior iliac spine
- Inferior attachment: pubis
- Courses obliquely in an inferomedial direction
- Sacrospinous ligament
- Attaches from the ischial spine to the lateral border of the sacrum
- Crosses in front of the sacrotuberous ligament, fusing with it medially
- Covered by the coccygeus muscle
- Above this lies the sciatic nerve and plexus, which is an important structure to avoid during vault suspensions.
- Sacrotuberous ligament
- Attaches from the ilium and ischium to the sacrum It runs from the posterior iliac spine along the sacral border and attaches to the ischial tuberosity
- The sacrospinous and sacrotuberous ligaments separate the sciatic foramen into the greater and lesser sciatic foramina [Chapter 68 suggests only sacrospinous but Chapter 67 only mentions sacrotuberous and Wikipedia says both]
- Sacroiliac ligaments
- The short and long dorsal sacroiliac ligaments are posterior and connect the sacrum to the ilium.
- Vesicopelvic ligament or fascia
- Formed from fusion of the perivesical and endopelvic fascia.
- The transversalis fascia is part of the outer stratum and is continuous with the endopelvic and lateral pelvic fascia
- Formed from fusion of the perivesical and endopelvic fascia.
- Pubovesical/puboprostatic ligaments (pubourethral ligament)
- Puboprostatic in males; pubovesical in females
- Run from the pubic bone to the prostate/bladder neck
- Important structure in retropubic suspension since they hold the bladder neck in place when it contracts, and they provide a hammocklike support to the mid-urethra.
- Inguinal ligament
- Muscles of the pelvic floor
- Pelvic sidewalls
- Formed by (6):
- Obturator internus
- Iliacus
- Psoas major
- Psoas minor
- Levator ani system
- Coccygeus
- Formed by (6):
- Pelvic floor
- Formed by (2):
- Pelvic diaphragm, which extends from the pubis anteriorly to the coccyx posteriorly
- Levator ani muscles, which plays an important role in support of the urogenital viscera as well as their function.
- The levator ani complex consists of (3):
- Pubococcygeus
- Puborectalis
- Iliococcygeus
- The name of each of its components is derived from their attachments.
- The levator ani complex consists of (3):
- Formed by (2):
- Pelvic sidewalls
Pelvic Vasculature[edit | edit source]
Arterial supply[edit | edit source]
- Abdominal aorta branches into:
- Middle sacral artery
- Arises posteriorly at the bifurcation of the aorta and travels on the pelvic surface of the sacrum
- Supplies branches to the sacral foramina and the rectum
- Paired common iliac arteries
- Arise at the level of the L4
- Run anterior and lateral to their accompanying veins
- Bifurcate into the external and internal iliac arteries at the SI joint.
- Middle sacral artery
External iliac artery[edit | edit source]
- Source: branch of the common iliac artery
- Location: Follows the medial border of the iliopsoas muscle along the arcuate line and leaves the pelvis beneath the inguinal ligament and continues as the femoral artery
- Surgical considerations
- Only vessel in the pelvis without adequate collateral circulation; if ligated will cause significant sequella
- Branch (1):
- Inferior epigastric artery§
- Source: branch of the external iliac artery
- Location
- Branches off of the external iliac artery proximal to the inguinal ligament and ascends medially along the anterior abdominal wall, medial to the internal inguinal ring; enveloped by lateral umbilical ligament
- Insert figure
- Hesselbach triangle borders (3):
- Lateral: inferior epigastric vessels
- Medial: rectus abdominus muscle
- Inferior: inguinal ligament
- Pierces transversalis fascia as it continues to ascend superiorly and superficially, until it levels posterior to rectus once is crosses the arcuate line/linea semicircularis. Continues to rise superiorly until it terminates by piercing rectus abdominis and branches and forms and anastamosis with the superior epigastric arteries, at approximately the level of the superior epigastric arteries.
- Branches (3):
- Deep circumflex iliac – supplies inguinal ligament and surrounding structures laterally (See Figure), can also arise directly from external iliac
- Pubic – supplies inguinal ligament and surrounding structures medially
- Cremesteric – supplies vas deferens and testis
- In 25% of people, an accessory obturator artery arises from the inferior epigastric artery and runs medial to the femoral vein to reach the obturator canal. This vessel must be avoided during obturator lymph node dissection
- Rectus muscle and overlying skin
- Surgical considerations
- Can be ligated without complication because the rectus is richly collateralized from above and laterally
- Inferior epigastric artery§
Internal iliac artery[edit | edit source]
- Also known as hypogastric artery
- Source: common iliac artery
- Location: Descends in front of the SI joint
- Branches (2): divides into an anterior and a posterior trunk approximately 3-4 cm from the bifurcation.
- Posterior trunk
- Surgical considerations
- Rarely seen during pelvic surgery
- Branches (3) S-GALLS
- Superior Gluteal
- Exits the greater sciatic foramen
- Supplies gluteus muscles and overlying skin
- Ascending Lumbar/iliolumbar
- Supplies the posterior abdominal wall (psoas and quadratus lumborum muscles and adjacent structures)
- Lateral Sacral
- Passes medially to join the middle sacral branches from the aorta at the sciatic foramina
- Supplies sacral nerves and sacrum
- Superior Gluteal
- Surgical considerations
- Anterior trunk
- Surgical considerations
- The primary branches identified during retroperitoneal surgery include the superior vesical artery, the uterine artery, and occasionally the obturator artery.
- Branches (6) Mr. U IPIG SVIVO
- Umbilical
- In fetus, paired arteries surroud bladder and extend into umbilical cord.
- After birth, a portion regresses to become the medial umbilical ligaments, while a portion remains open as the first branch off of the anterior trunk
- Obliterated umbilical artery is lateral to the ureter at the pelvic brim
- The open portion gives rises to the Superior Vesical artery
- Superior Vesical artery
- Surgical considerations
- Most prominent branch of the internal iliac artery and in most cases appears to be a continuation of it.
- Identification is possible with development of the paravesical space and during dissection of the obturator space.
- Supplies
- Bladder, ureter, vas deferens, and seminal vesicle
- Branch (1)
- Artery of the vas
- Supplies seminal vesicles and vas deferens
- Can also come off the umbilical artery or the inferior vesical artery.
- Travels the length of the vas to meet the cremasteric and testicular arteries distally. Because of these anastomoses, the testicular artery may be sacrificed without compromising the viability of the testis.
- Artery of the vas
- Surgical considerations
- Superior Vesical artery
- Obturator
- Variable in origin
- Travels through the obturator fossa medial and posterior to the obturator nerve
- Supplies adductor muscles of the thigh and overlying skin
- Inferior Vesical
- Supplies bladder base, seminal vesicle, prostate, lower ureter, and the neurovascular bundle
- Middle Rectal
- Gives small branches to the seminal vesicles and prostate and anastomoses with the inferior and superior rectal arteries in the rectal wall.
- Supplies rectum, ureter, and bladder
- Internal Pudendal
- Terminal branch of the internal iliac artery
- Location
- Leaves the pelvis through the greater sciatic foramen, passes around the sacrospinous ligament, and enters the lesser sciatic foramen to gain access to the perineum.
- After entering the perineum through the lesser sciatic foramen, the artery runs in a fascial sheath on the medial aspect of obturator internus, which is the pudendal canal (of Alcock).
- Branches (5): IPP BC
- Inferior rectal artery
- Perineal artery
- Posterior scrotal/labial
- Artery of Bulb of penis
- Common penile artery (terminal branch)
- The common penile artery branches into the (3):
- Cavernosal artery
- Bulbourethral artery
- Dorsal artery
- The common penile artery branches into the (3):
- Supplies rectum, perineum, and external genitalia
- Note that the external pudendal artery comes from the femoral artery and the superior rectal artery comes from the inferior mesenteric artery
- Inferior Gluteal
- Travels through the greater sciatic foramen
- Supplies gluteus muscles and overlying skin
- Vaginal (if female)
- Uterine (if female)
- Often branches off of superior vesical artery
- Passes anterior to ureter and enters the lateral uterus at the level of the internal cervical os to meet ovarian artery
- Umbilical
- Surgical considerations
- Posterior trunk
Venous drainage[edit | edit source]
Internal iliac vein[edit | edit source]
- Joined by tributaries corresponding to the branches of the internal iliac artery
- Ascends medial and posterior to the artery
- Relatively thin walled and at risk for injury during dissection of the artery or the nearby pelvic ureter
External iliac vein[edit | edit source]
- A continuation of the femoral vein
- Ascends medial and posterior to its artery
- Joins the internal iliac vein behind the internal iliac artery
- Drains the inferior epigastric vein, deep circumflex iliac, and pubic veins
- In 50% of patients, one or more accessory obturator veins drain into the underside of the external iliac vein and can be easily torn during lymphadenectomy
Pelvic Lymphatics[edit | edit source]
- The pelvic lymph nodes can be difficult to appreciate on gross examination because they are embedded in the fatty and fibrous tissue of the intermediate stratum.
Pelvic Innervation[edit | edit source]
Somatic nerves of the lower abdomen and pelvis
| Nerve | Origin | Motor | Sensory |
| Iliohypogastric | L1 | Internal oblique and transversus muscles | Lower anterior abdominal wall |
| Ilioinguinal | L1 | Anterior scrotum (or mons pubis and labium majus), root of penis, and upper medial thigh | |
| Genitofemoral | L1, L2 | Genital branch: cremaster muscle | Genital branch: anterior scrotum (or mons pubis and labium majus)
Femoral branch: upper anterior thigh |
| Lateral femoral cutaneous nerve of thigh | L2, L3 | Sensory to anterior and lateral thigh | |
| Femoral | L2, L3, L4 | Extensors of the knee | Anterior thigh and medial leg |
| Obturator | L2, L3, L4 | ADDuctors of the thigh | Medial thigh |
| Lumbosacral trunk | L4, L5 | Joins the sacral nerves to form the lumbosacral plexus that supplies motor and
sensory innervation to the lower extremities | |
| Posterior femoral cutaneous | S2, S3 | Perineum, posterior scrotum, and posterior thigh | |
| Pudendal | S2, S3, S4 | Levator ani, muscles of the urogenital diaphragm, anal and striated urethral sphincter | Perineum, scrotum, penis |
| Pelvic somatic efferents | S2, S3, S4 | Motor supply to levator ani and striated urethral sphincter | |
| Nervi erigentes | S2, S3, S4 | Parasympathetic fibers from the sacral cord that supply the pelvic viscera | |
- Lumbosacral plexus
- The ilioinguinal and iliohypogastric nerves run laterally over the anterior aspect of the quadratus lumborum and travel through the transversus abdominis to run deep to the internal oblique muscle
- The ilioinguinal nerve (L1) passes through the internal oblique muscle to enter the inguinal canal laterally. This nerve travels outside and anterior to the cord. Can be damaged during orchiectomy
- Genitofemoral nerve (L1, L2)
- Courses anterior and parallel to the psoas muscle and pierces the psoas muscle to reach its anterior surface in the retroperitoneum and then travels to the pelvis
- May be injured during a psoas hitch procedure (suture placement) and laparoscopic varicocelectomy (ligation).
- The nerve typically divides into genital and femoral branches near the level of the inguinal ligament.
- The genital branch travels IN the spermatic cord through the inguinal canal.
- The femoral branch passes under the inguinal ligament and enters the femoral sheath.
- Lateral femoral cutaneous nerve of thigh
- Lateral to psoas muscle in iliacus fascia
- Femoral nerve (L2, L3, L4)
- Travels within the psoas muscle for most of its pelvic course and then exits its lateral side to pass under the inguinal ligament.
- During a psoas hitch, sutures should be placed in the direction of the nerve (and the psoas muscle fibers) to avoid nerve damage or entrapment.
- Compression of the femoral nerve may occur intraoperatively with placement of retractor blades on the psoas muscle or inferolaterally against the inguinal ligament
- A stretch injury to the femoral nerve may occur with prolonged hip flexion in low lithotomy position used during minimally invasive pelvic surgery
- Obturator nerve (L2, L3, L4)
- Emerges in the true pelvis from beneath the psoas muscle, lateral to the internal iliac vessels, and passes through the obturator fossa to the obturator canal. In the fossa, it is lateral and superior to the obturator vessels and is surrounded by the obturator and internal iliac lymph nodes.
- Electrocautery employed during a transurethral resection of bladder tumor (TURBT) procedure may result in obturator nerve stimulation with subsequent rapid, forceful hip adduction. If this potential event is not anticipated and accounted for, severe bladder perforation may occur
- An exaggerated lithotomy position may stretch the lumbosacral nerve (L4, L5) or place pressure on its peroneal branch (L4-S2, terminal branch of sciatic nerve) at the fibular head to produce foot drop.
- The sacral plexus lies on pelvic surface of piriformis deep to endopelvic fascia & posterior to internal iliac vessels
- Pelvic and perineal branches of the sacral plexus include (4):
- The posterior femoral cutaneous nerve (S2, S3)
- The pudendal nerve (S2, S3, S4)
- The nervi erigentes (S2, S3, S4) to the autonomic plexus
- Pelvic somatic efferent nerves from the ventral rami of S2, S3, and S4, which travel on the pelvic surface of the levator ani in close association with the rectum and prostate and are separated from the pelvic autonomic plexus by the endopelvic fascia.
- Pudendal nerve
- Follows the internal pudendal artery to the perineum
- Branches (3):
- Dorsal nerve of penis/clitoris (first branch)
- Inferior rectal nerve
- Perineal nerve
- The ilioinguinal and iliohypogastric nerves run laterally over the anterior aspect of the quadratus lumborum and travel through the transversus abdominis to run deep to the internal oblique muscle
- Autonomic Innervation
- Pelvic/Inferior hypogastric plexus
- The presynaptic sympathetic cell bodies reach the pelvic plexus by 2 pathways:
- Superior hypogastric plexus
- Cell bodies in the lateral column of gray matter from T10-L2 which project to the pelvic autonomic plexus [via the hypogastric nerve]
- Pelvic continuation of the sympathetic trunks
- Branches from the sacral sympathetic ganglia
- Superior hypogastric plexus
- Pre-synaptic parasympathetic innervation arises from the intermediolateral cell column of the S2-4 (pelvic splanchnic nerves/nervi erigentes) sacral cord
- Rectangular, ≈4-5 cm long, and its midpoint is at the tips of the seminal vesicles.
- Oriented in the sagittal plane on either side of the rectum
- Pierced by the numerous vessels going to and from the rectum, bladder, seminal vesicles, and prostate.
- Clinical significance: Division of the so-called lateral pedicles of the bladder and prostate proximally not only interrupts the vessels but also transects the nerve supply to the prostate, urethra, and corpora cavernosa with attendant postoperative impotence. Ligation is best carried out near the bladder to avoid nerve damage.
- During radical prostatectomy, the nerves are most vulnerable at the apex of the prostate, where they closely approach the prostatic capsule at the 5 and 7 o’clock positions.
- The presynaptic sympathetic cell bodies reach the pelvic plexus by 2 pathways:
- Pelvic/Inferior hypogastric plexus
Rectum[edit | edit source]
- Peritoneum continues anteriorly over the upper two thirds of the rectum as the rectovesical pouch in males
- Inferior to this pouch, the anterior rectum is related to its fascial continuation (the rectogenital or Denonvilliers fascia) down to the level of the striated urethral sphincter
- Anterior fibers of outer longitudinal smooth muscles of colon leave the rectum to join posterior external urinary sphincter forming the rectourethralis muscle
- Blood supply:
- Superior rectal artery (from IMA)
- Middle rectal artery (from internal iliac)
- Inferior rectal artery (from internal pudendal)
Pelvic ureter[edit | edit source]
- See Ureter Anatomy Chapter Notes
- Intraoperatively the ureter is readily found anterior to the bifurcation of the common iliac artery
- The ureters come within 5 cm of each other as they cross the iliac vessels. On entering the pelvis, they diverge widely along the pelvic sidewalls toward the ischial spines. The ureter travels on the anterior surface of the internal iliac vessels and is related laterally to the branches of the anterior trunk. Near the ischial spine, the ureter turns anteriorly and medially to reach the bladder.
- In men, the anteromedial surface of the ureter is covered by the peritoneum, and the ureter is embedded in retroperitoneal connective tissue.
- As the ureter courses medially, it is crossed anteriorly by the vas deferens and runs with the inferior vesical arteries, veins, and nerves in the lateral vesical ligaments. Viewed from the peritoneal side, the ureter is just lateral and deep to the rectogenital fold
- Structures divided in order to access the distal ureter in females (5):
- Round ligament
- Obliterated umbilical artery
- Uterine artery
- Superior vesical artery
- Inferior vesical artery
Perineum[edit | edit source]
- The perineum lies between the pubis, thighs, and buttocks and is limited superiorly by the levator ani.
- Viewed from below, the symphysis pubis, ischial tuberosities, and coccyx outline the diamond shape of the perineum; the inferior ischiopubic rami and sacrotuberous ligaments form its bony and ligamentous walls. A line drawn through the ischial tuberosities divides the perineum into an anal and a urogenital triangle.
- Perineal membrane (previously called the urogenital diaphragm)
- A sheet of fascia that lies between the two sides of the pubic arch.
- Divides the urogenital hiatus into:
- Superficial perineal space
- Deep perineal space
- Male urogenital triangle
- Borders are pubic symphysis, ischial spines laterally, and perineal body and transverse perinei muscles
- The scrotum hangs from the anterior aspect of the urogenital triangle; in the posterior aspect, skin and subcutaneous fat overlie Colles fascia.
- The perineal membrane and the posterior and lateral attachments of Colles fascia limit a potential space known as the superficial pouch.
- In this superficial pouch, the 3 erectile bodies of the penis have their bony and fascial attachments (the root of the penis).
- The paired corpora cavernosa attach to the inferior ischiopubic rami and perineal membrane and are surrounded by the ischiocavernosus muscles.
- The corpus spongiosum dilates proximally as the bulb of the penis and is fixed to the center of the perineal membrane. It is encompassed by the bulbospongiosus muscles that arises from the perineal body and from a central tendinous raphe and pass around the bulb to attach to the perineal membrane and dorsum of the penis. Contraction of the ischiocavernosus and bulbospongiosus muscles compresses the erectile bodies and potentiates penile erection.
- Blood supply to the anal and urogenital triangles is derived largely from the internal pudendal vessels.
- The internal pudendal veins communicate freely with the dorsal vein complex by piercing the levator ani.
- The pudendal nerve follows the vessels in their course through the perineum. Its first branch, the dorsal nerve of the penis, travels ventral to the main pudendal trunk in Alcock canal.
- Perineal lymphatics
- The penis, scrotum, and perineum drain into the inguinal lymph nodes.
- These inguinal lymph nodes may be divided into a superficial and a deep group, which are separated by the deep fascia of the thigh (fascia lata).
- Scrotal lymphatics DON’T cross median raphe and drain into ipsilateral superficial inguinal nodes only, whereas penile lymphatics can cross over and drain to superficial and deep inguinal nodes
- The penis, scrotum, and perineum drain into the inguinal lymph nodes.
Questions[edit | edit source]
Answers[edit | edit source]
References[edit | edit source]
- Kandinata, Natalie, and Kelly Van Fossen."Anatomy, Abdomen and Pelvis, Epigastric Artery." (2019).
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 68