Normal Erectile Physiology: Difference between revisions
Jump to navigation
Jump to search
Urology4all (talk | contribs) |
Urology4all (talk | contribs) |
||
| (5 intermediate revisions by the same user not shown) | |||
| Line 38: | Line 38: | ||
=== Neurotransmitters === | === Neurotransmitters === | ||
==== Nitric oxide ==== | |||
* '''<span style="color:#ff0000">Principal neurotransmitter mediating erection</span>''' | |||
* '''<span style="color:#ff0000">Synthesized by nitric oxide synthase (NOS)</span>''' | |||
** '''<span style="color:#ff0000">Nitric oxide synthase</span>''' | |||
*** '''<span style="color:#ff0000">3 isoforms; all 3 have been identified in the corpus cavernosum:</span>''' | |||
***# '''<span style="color:#ff0000">Neuronal nitric oxide synthase (</span><span style="color:#0000ff">n</span><span style="color:#ff0000">NOS) in the nitrergic nerves: responsible for the i</span><span style="color:#0000ff">NNN</span><span style="color:#ff0000">itiation</span>''' | |||
***# '''<span style="color:#ff0000">Endothelial nitric oxide synthase (</span><span style="color:#0000ff">e</span><span style="color:#ff0000">NOS): contributes to the maint</span><span style="color:#0000ff">EEE<span style="color:#ff0000">nance of smooth muscle relaxation and erection</span>''' | |||
***# '''<span style="color:#0000ff">i</span><span style="color:#ff0000">NOS</span>''' | |||
* '''<span style="color:#ff0000">Released from (2):</span>''' | |||
*# '''<span style="color:#ff0000">Non-adrenergic/non-cholinergic (NANC) neurotransmission from postganglionic parasympathetic stimulation [from the cavernous nerves]</span>''' | |||
*# '''<span style="color:#ff0000">Endothelium</span>''' | |||
* '''<span style="color:#ff0000">Stimulates production of cGMP from GMP</span>''' by activating guanylate cyclase in smooth muscle | |||
**'''<span style="color:#ff0000">Increased cGMP results in smooth muscle relaxation</span>''' by activating cGMP-dependent protein kinases, which phosphorylate certain proteins and ion channels, resulting in: | |||
**# Opening of the potassium channels and hyperpolarization | |||
**# Sequestration of intracellular calcium by the endoplasmic reticulum | |||
**# Inhibition of voltage-dependent calcium channels, blocking calcium influx | |||
* '''<span style="color:#ff0000">The smooth muscle regains its tone when cGMP is degraded by phosphodiesterase</span>''' | |||
* | |||
===== '''<span style="color:#ff0000">Phosphodiesterase (PDE)</span>''' ===== | |||
* '''<span style="color:#ff0000">Enzyme that degrades cGMP to GMP</span>''' | |||
*11 subtypes | |||
** '''All subtypes, except PDE6 which is specifically expressed in photoreceptor cells, have been identified in the corpus cavernosum''' | |||
** '''<span style="color:#ff0000">PDE5 is the principal PDE for the termination of cavernous cGMP signaling</span>''' | |||
* ''' | ==== '''Others''' ==== | ||
*'''Neurotransmitters that promote sexual function: dopamine, acetylcholine, oxytocin, and serotonin (5-HT)''' | |||
** '''Acetylcholine contributes indirectly to penile erection''' by presynaptic stimulation of NO release from endothelial cells and inhibition of adrenergic neurons which decreases the release of norepinephrine | ** '''Acetylcholine contributes indirectly to penile erection''' by presynaptic stimulation of NO release from endothelial cells and inhibition of adrenergic neurons which decreases the release of norepinephrine | ||
* '''Norepinephrine is the principal neurotransmitter mediating flaccidity''' | * '''Norepinephrine is the principal neurotransmitter mediating flaccidity''' | ||
| Line 84: | Line 85: | ||
**6, slow detumescence | **6, slow detumescence | ||
**7, fast detumescence | **7, fast detumescence | ||
==== '''<span style="color:#ff0000">Flaccid state''' ==== | |||
*'''<span style="color:#ff0000">In contrast to many other smooth muscles, the cavernous smooth muscle and the smooth muscles of the arteriolar and arterial wall are in a contracted state most of the time, allowing only a small amount of arterial flow into the corpora.''' | |||
** '''Maintenance of the intracorporeal smooth muscle in a semicontracted (flaccid) state likely results from 3 factors:''' | |||
**# '''Intrinsic myogenic activity''' | |||
**# '''Adrenergic neurotransmission''' | |||
**# '''Endothelium-derived contracting factors such as angiotensin II, PGF2α, and endothelin-1''' | |||
** Smooth muscle has the ability to maintain tension for prolonged periods with minimal energy expenditure. This efficiency has been termed the latch state and is critical for sustaining the "basal" tone of the smooth muscle. | |||
==== '''<span style="color:#ff0000">Transition to erection/tumescence</span>''' ==== | |||
*'''<span style="color:#ff0000">Sexual stimulation triggers release of neurotransmitters from the parasympathetic cavernous nerve terminals.</span>''' | |||
*'''This release of neurotransmitters (see above) results in relaxation of these smooth muscles and the following events:''' | |||
*# '''Dilation of the arterioles and arteries''' by increasing blood flow in the diastolic and systolic phases | |||
*# Trapping of the incoming blood by the expanding sinusoids | |||
*# '''Compression of the subtunical venous plexuses''' between the tunica albuginea and the peripheral sinusoids, '''decreasing venous outflow''' | |||
*# Stretching of the tunica to its capacity, which '''occludes the emissary veins''' between the inner circular and outer longitudinal layers and further decreases venous outflow | |||
*# '''Increase in PO2 (≈90 mm Hg) and intracavernous pressure (≈100 mm Hg),''' which raises the penis from the dependent position to the erect state (the full erection phase). | |||
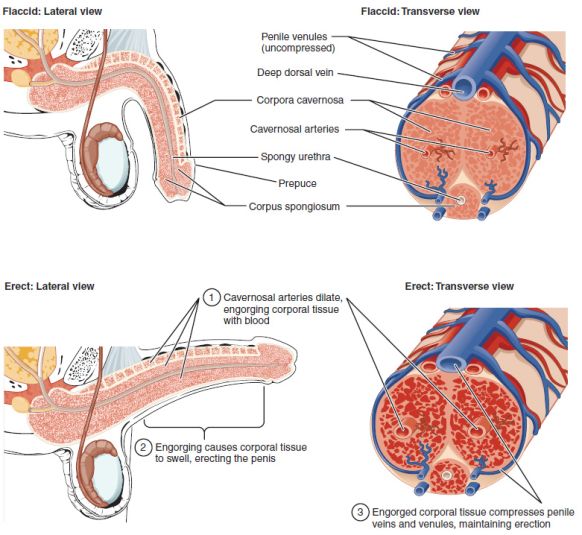
* '''Erection involves sinusoidal relaxation, arterial dilation (increased inflow), and venous compression (decreased outflow)''' | |||
*See [[commons:File:Erection_Development.jpg|Figure demonstrating the development of an erection]] | |||
[[File:Figure 28 01 06.jpg|alt=Anatomic representation of changes to penis during erection.|thumb|582x582px|Anatomic representation of changes to penis during erection. Source: [[commons:File:Figure_28_01_06.jpg|Wikipedia]]|center]] | |||
==== '''<span style="color:#ff0000">Transition to detumescence</span>''' ==== | |||
*'''<span style="color:#ff0000">3 phases of detumescence:</span>''' | |||
*# '''<span style="color:#ff0000">Transient intracorporeal pressure increase, indicating the beginning of smooth muscle contraction against a closed venous system</span>''' | |||
*# '''<span style="color:#ff0000">Slow pressure decreases</span>''', suggesting a slow reopening of venous channels with resumption of the basal level of arterial flow | |||
*# '''<span style="color:#ff0000">Fast pressure decrease</span>''' with fully restored venous outflow capacity | |||
*'''<span style="color:#ff0000">Detumescence after erection may be a result of (3):</span>''' | |||
*# '''<span style="color:#ff0000">Cessation of NO release</span>''' | |||
*# '''<span style="color:#ff0000">Breakdown of cGMP by PDEs</span>''' | |||
*# '''<span style="color:#ff0000">and/or sympathetic discharge during ejaculation</span>''' | |||
=== Corpus spongiosum and glans penis === | === Corpus spongiosum and glans penis === | ||
* '''During erection, the arterial flow increases in a similar manner; however, the pressure in the corpus spongiosum and glans is only 1/3-1/2 that in the corpora cavernosa because the spongiosum lacks the outer longitudinal layer of the tunica albuginea,''' resulting in minimal venous occlusion (Chapter 26 suggests tunica albuginea absent from corpus spongiosum but Chapter 21 specifies that outer longitudinal layer is absent) | * '''During erection, the arterial flow increases in a similar manner; however, the pressure in the corpus spongiosum and glans is only 1/3-1/2 that in the corpora cavernosa because the spongiosum lacks the outer longitudinal layer of the tunica albuginea,''' resulting in minimal venous occlusion (Chapter 26 suggests tunica albuginea absent from corpus spongiosum but Chapter 21 specifies that outer longitudinal layer is absent) | ||
Latest revision as of 20:10, 20 March 2024
See Penis Anatomy Chapter Notes
Neuroanatomy and Neurophysiology of Penile Erection[edit | edit source]
Spinal centers and peripheral pathways[edit | edit source]
- Neural pathways necessary for complete sexual function:
- Autonomic
- Parasympathetic
- Sympathetic
- Somatic (sensory and motor)
- Autonomic
Autonomic[edit | edit source]
- Parasympathetic (lateral horns S2-S4)
- Responsible for tumescence (increasing rigidity)
- The parasympathetic preganglionic fibers pass in the pelvic splanchnic nerves to the inferior hypogastric plexus (also known as the pelvic plexus)
- Sympathetic (lateral horns T10-L2)[1]
- Responsible for detumescence (decreasing rigidity)
- The lumbar sympathetics from the superior hypogastric plexus (in older texts, hypogastric plexus or presacral nerve) travel to the inferior hypogastric plexus via the hypogastric nerve
- The sympathetic postganglionic fibers pass in the sacral splanchnic nerves from the sympathetic chain to the inferior hypogastric plexus
- The sympathetic and parasympathetic nerves merge in the inferior hypogastric/pelvic plexus to form the paired cavernous nerves, which enter the corpora cavernosa and corpus spongiosum and innervate the penis
- Clinical implication: nerve-sparing prostatectomy aims to avoid injury to the cavernous nerves.
Somatic[edit | edit source]
- Center of somatomotor penile innervation (also motorneurons for external urinary sphincter) is in S2-S4 spinal cord region and is called Onuf's nucleus
- Onuf nucleus (S2-S4)
- Nerve fibers from neurons in Onuf's nucleus travel in the sacral nerves to become the pudendal nerve (S2-S4).
- Pudendal nerve
- A mixed nerve (both sensory and motor components)
- Throughout most of its path, the nerve is closely associated with the branches of the internal pudendal artery and vein.[2]
- Responsible for (3):
- Penile sensation
- The nerve fibers from the sensory receptors in the penile skin, glans, and urethra and within the corpus cavernosum converge to form bundles of the dorsal nerve of the penis, which joins other nerves to become the pudendal nerve
- Contraction of the ischiocavernosus muscle
- Produces the rigid-erection phase
- Contraction of the bulbocavernosus/bulbospongiosus muscles (and external urethral sphincter)
- Rhythmic contraction and compression on the proximal corpus spongiosum helps expel semen
- Penile sensation
- Enters the spinal cord via the S2-S4 roots to terminate on spinal neurons and interneurons in the central gray region of the lumbosacral segment. Activation of these sensory neurons sends messages of pain, temperature, and touch by means of spinothalamic and spinoreticular pathways to the thalamus and sensory cortex for sensory perception
Neurotransmitters[edit | edit source]
Nitric oxide[edit | edit source]
- Principal neurotransmitter mediating erection
- Synthesized by nitric oxide synthase (NOS)
- Nitric oxide synthase
- 3 isoforms; all 3 have been identified in the corpus cavernosum:
- Neuronal nitric oxide synthase (nNOS) in the nitrergic nerves: responsible for the iNNNitiation
- Endothelial nitric oxide synthase (eNOS): contributes to the maintEEEnance of smooth muscle relaxation and erection
- iNOS
- 3 isoforms; all 3 have been identified in the corpus cavernosum:
- Nitric oxide synthase
- Released from (2):
- Non-adrenergic/non-cholinergic (NANC) neurotransmission from postganglionic parasympathetic stimulation [from the cavernous nerves]
- Endothelium
- Stimulates production of cGMP from GMP by activating guanylate cyclase in smooth muscle
- Increased cGMP results in smooth muscle relaxation by activating cGMP-dependent protein kinases, which phosphorylate certain proteins and ion channels, resulting in:
- Opening of the potassium channels and hyperpolarization
- Sequestration of intracellular calcium by the endoplasmic reticulum
- Inhibition of voltage-dependent calcium channels, blocking calcium influx
- Increased cGMP results in smooth muscle relaxation by activating cGMP-dependent protein kinases, which phosphorylate certain proteins and ion channels, resulting in:
- The smooth muscle regains its tone when cGMP is degraded by phosphodiesterase
Phosphodiesterase (PDE)[edit | edit source]
- Enzyme that degrades cGMP to GMP
- 11 subtypes
- All subtypes, except PDE6 which is specifically expressed in photoreceptor cells, have been identified in the corpus cavernosum
- PDE5 is the principal PDE for the termination of cavernous cGMP signaling
Others[edit | edit source]
- Neurotransmitters that promote sexual function: dopamine, acetylcholine, oxytocin, and serotonin (5-HT)
- Acetylcholine contributes indirectly to penile erection by presynaptic stimulation of NO release from endothelial cells and inhibition of adrenergic neurons which decreases the release of norepinephrine
- Norepinephrine is the principal neurotransmitter mediating flaccidity
- α-Adrenergic nerve fibers and receptors are present in cavernous trabeculae and surrounding the cavernous arteries.
- GABAb receptors inhibit erectile function
- Prostaglandin E1 is erectogenic, intracavernous injection of PGE1 is one of the safest and most effective treatments for ED
- Sonic hedgehog has been identified in the penis; inhibition of SHH in adult rats leads to rapid atrophy and disorganization of the corpus cavernosum. SHH has been shown to stimulate the expression of vascular endothelial growth factor (VEGF) and NOS in the penis
- Cannabinoid CB1 receptor activation inhibits sexual function by modulating the paraventricular oxytocinergic neurons, which mediate erection. Antagonism of CB1 receptors in the PVN of male rats induces penile erection
Hemodynamics and Mechanisms of Erection and Detumescence[edit | edit source]
Corpora cavernosa[edit | edit source]
- 7 phases of erection/detumesence:
- 0, flaccid
- 1, latent
- 2, tumescence
- 3, full erection
- 4, rigid erection
- 5, initial detumescence
- 6, slow detumescence
- 7, fast detumescence
Flaccid state[edit | edit source]
- In contrast to many other smooth muscles, the cavernous smooth muscle and the smooth muscles of the arteriolar and arterial wall are in a contracted state most of the time, allowing only a small amount of arterial flow into the corpora.
- Maintenance of the intracorporeal smooth muscle in a semicontracted (flaccid) state likely results from 3 factors:
- Intrinsic myogenic activity
- Adrenergic neurotransmission
- Endothelium-derived contracting factors such as angiotensin II, PGF2α, and endothelin-1
- Smooth muscle has the ability to maintain tension for prolonged periods with minimal energy expenditure. This efficiency has been termed the latch state and is critical for sustaining the "basal" tone of the smooth muscle.
- Maintenance of the intracorporeal smooth muscle in a semicontracted (flaccid) state likely results from 3 factors:
Transition to erection/tumescence[edit | edit source]
- Sexual stimulation triggers release of neurotransmitters from the parasympathetic cavernous nerve terminals.
- This release of neurotransmitters (see above) results in relaxation of these smooth muscles and the following events:
- Dilation of the arterioles and arteries by increasing blood flow in the diastolic and systolic phases
- Trapping of the incoming blood by the expanding sinusoids
- Compression of the subtunical venous plexuses between the tunica albuginea and the peripheral sinusoids, decreasing venous outflow
- Stretching of the tunica to its capacity, which occludes the emissary veins between the inner circular and outer longitudinal layers and further decreases venous outflow
- Increase in PO2 (≈90 mm Hg) and intracavernous pressure (≈100 mm Hg), which raises the penis from the dependent position to the erect state (the full erection phase).
- Erection involves sinusoidal relaxation, arterial dilation (increased inflow), and venous compression (decreased outflow)
- See Figure demonstrating the development of an erection
Transition to detumescence[edit | edit source]
- 3 phases of detumescence:
- Transient intracorporeal pressure increase, indicating the beginning of smooth muscle contraction against a closed venous system
- Slow pressure decreases, suggesting a slow reopening of venous channels with resumption of the basal level of arterial flow
- Fast pressure decrease with fully restored venous outflow capacity
- Detumescence after erection may be a result of (3):
- Cessation of NO release
- Breakdown of cGMP by PDEs
- and/or sympathetic discharge during ejaculation
Corpus spongiosum and glans penis[edit | edit source]
- During erection, the arterial flow increases in a similar manner; however, the pressure in the corpus spongiosum and glans is only 1/3-1/2 that in the corpora cavernosa because the spongiosum lacks the outer longitudinal layer of the tunica albuginea, resulting in minimal venous occlusion (Chapter 26 suggests tunica albuginea absent from corpus spongiosum but Chapter 21 specifies that outer longitudinal layer is absent)
Types of Erections (3):[edit | edit source]
- Psychogenic erection:
- Reflexogenic erection:
- Result of tactile stimulation of the genital organs
- The impulses reach the spinal erection centers (T11-L2 and S2-S4); some then follow the ascending tract, resulting in sensory perception, whereas others activate the autonomic nuclei to send messages via the parasympathetic cavernous nerves to the penis to induce erection.
- Reflexogenic erection is preserved in 95% of patients with complete upper cord lesions [above S2] but in only about 25% of patients with complete lower cord lesions
- Nocturnal erection:
- Occurs mostly during rapid eye movement (REM) sleep
Spinal cord injury level and erections[edit | edit source]
- Above T10 (some sources T11), get reflex only
- Below L2 but above S2: both
- S2 or below: psychogenic (but not as strong)
Ejaculation[edit | edit source]
Questions[edit | edit source]
- Explain the physiology of an erection
- Why does the corpus spongiosum not become as rigid as the corpora cavernosae?
- Describe the autonomic innervation and somatic involved in erection?
- What is the main neurotransmitter involved in erection? Where is it released from? What is its function? What enzyme synthesizes it? Which enzyme subtype is responsible for initiation vs. maintenance of erection?
- What is the principal neurotransmitter involved in detumesence?
- Which phosphodiesterase subtypes are found in the corpus cavernosum? Which subtype is the main one mediating detumescence?
- What are the phases of detumescence?
- What are the 3 types of erection? Which is most likely preserved on a patient with upper spinal cord injury?
Answers[edit | edit source]
- Explain the physiology of an erection
- In the flaccid state, the cavernous smooth muscle and the smooth muscles of the arteriolar and arterial wall are tonically contracted, allowing only a small amount of arterial flow into the corpora
- Sexual stimulation triggers release of neurotransmitters from the cavernous nerve terminals. This release of neurotransmitters results in relaxation of these smooth muscles results in
- Increased blood inflow
- Decreased blood outflow
- Increase in PO2 and intracavernous pressure
- Why does the corpus spongiosum not become as rigid as the corpora cavernosae?
- The corpus spongiosum lacks the outer longitudinal layer of the tunica albuginea
- Describe the autonomic innervation and somatic involved in erection?
- Parasympathetic (S2-S4): erection
- Sympathetic (T10-T12): detumesence, emission
- Somatic (S2-S4, Onuf nucleus): pudendal nerve is responsible for sensation and contraction of the ischiocavernosus and bulbocavernosus/bulbospongiosus muscles (and external urethral sphincter)
- What is the main neurotransmitter involved in erection? Where is it released from? What is its function? What enzyme synthesizes it? Which enzyme subtype is responsible for initiation vs. maintenance of erection?
- Nitric oxide
- Non-adrenergic, non-cholinergic nerve terminals and the endothelium
- Stimulate production of cGMP by activation guanylate cyclase in smooth muscle; increased cGMP in smooth muscle stimulates relaxation
- Nitric oxide synthase; nNOS for initiation, eNOS for maintenance
- What is the principal neurotransmitter involved in detumesence?
- Norepinephrine
- Which phosphodiesterase subtypes are found in the corpus cavernosum? Which subtype is the main one mediating detumescence?
- All except PDE6, which is exclusively in the photoreceptors of the eye
- PDE5
- What are the phases of detumescence?
- What are the 3 types of erection? Which is most likely preserved on a patient with upper spinal cord injury?
- Nocturnal, psychologic, and reflexogenic
- Reflexogenic
Next Chapter: Pathophysiology of Erectile Dysfunction[edit | edit source]
References[edit | edit source]
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 26