Upper Urinary Tract Urothelial Cancer: Difference between revisions
Jump to navigation
Jump to search
Urology4all (talk | contribs) |
Urology4all (talk | contribs) |
||
| (94 intermediate revisions by the same user not shown) | |||
| Line 2: | Line 2: | ||
Includes 2023 AUA Upper Tract Urothelial Carcinoma Guideline Notes | Includes 2023 AUA Upper Tract Urothelial Carcinoma Guideline Notes | ||
See [https://www.youtube.com/watch?v=YQksUO0zoLc Video Review of 2023 AUA Guidelines on Upper Tract Urothelial Cancer] | |||
== Background == | |||
* UTUC refers to urothelial tumors that originate from the inner lining of the ureter, calyces, or renal pelvis | |||
* '''Definition of panurothelial disease:''' '''disease involving the bladder and 2 extravesical sites''' | |||
** In males, this could include one or both upper urinary tracts and/or the prostatic urethra | |||
** In females, this could be the bladder and both upper urinary tracts. | |||
** Low incidence and the lack of prospective studies do not permit absolute conclusions about treatment impact and outcomes | |||
== Epidemiology == | == Epidemiology == | ||
| Line 8: | Line 18: | ||
** Relatively rare | ** Relatively rare | ||
** US | ** US | ||
***Incidence: 2/100,000 | ***Incidence: rate 2/100,000 person-years, 7,000 cases/year | ||
**** '''<span style="color:#ff0000">Tumors of the renal pelvis are slightly more common than ureteral tumors</span>[https://seer.cancer.gov]''' | **** '''<span style="color:#ff0000">Tumors of the renal pelvis are slightly more common than ureteral tumors</span>[https://seer.cancer.gov]''' | ||
***** Renal pelvis: 1.2/100,000 | ***** Renal pelvis: 1.2/100,000 person-years | ||
***** Ureter: 0.8/100,000 | ***** Ureter: 0.8/100,000 person-years | ||
****** '''<span style="color:#ff0000">Ureteral tumours occur more commonly in the lower ureter (70%)</span> than in the upper ureter (25% mid, 5% upper).''' | ****** '''<span style="color:#ff0000">Ureteral tumours occur more commonly in the lower ureter (70%)</span> than in the upper ureter (25% mid, 5% upper).''' | ||
*******'''This may be a reflection of downstream implantation.''' | *******'''This may be a reflection of downstream implantation.''' | ||
| Line 19: | Line 29: | ||
*** '''Presentation at age <60 should raise concern of hereditary UTUC as part of Lynch syndrome''' | *** '''Presentation at age <60 should raise concern of hereditary UTUC as part of Lynch syndrome''' | ||
* '''Gender''' | * '''Gender''' | ||
** '''M:F | ** '''M:F 2:1 (unlike bladder which is M:F 4:1)[https://seer.cancer.gov/statistics-network/explorer/application.html]''' | ||
* Race | * Race | ||
** Whites are 2x more likely than Blacks to develop UTUC | ** Whites are 2x more likely than Blacks to develop UTUC | ||
== | == Risk Factors == | ||
=== <strong><span style="color:#ff0000">Hereditary (1)</span></strong> === | |||
# <strong><span style="color:#ff0000">[[Lynch syndrome]] (hereditary nonpolyposis colorectal carcinoma (HNPCC))</span></strong> | |||
#* <strong>Compared with non-hereditary cancers, patients are younger (mean age 55 years) and are more likely to be female</strong> | |||
=== <span style="color:#ff0000">Acquired (8)</span> === | |||
* '''<span style="color:#ff0000">Risk factors shared with bladder cancer (7)</span>''' | |||
*# '''<span style="color:#ff0000">Cigarette smoking</span>''' | |||
*#* '''<span style="color:#ff0000">Most important modifiable risk factor for UTUC</span>''' | |||
*#* Smoking cessation decreases subsequent risk | |||
*# '''<span style="color:#ff0000">Occupational exposure</span>''' | |||
*#* '''Exposure to aromatic hydrocarbons''', especially those used in the chemical, petrol, and plastic industries; other occupations at risk are those with exposure to coal, asphalt, or tar | |||
*# '''<span style="color:#ff0000">Chronic inflammation, infection, or iatrogenesis</span>''' | |||
*#* Chronic bacterial infection associated with urinary stones and obstruction has been associated with the development of squamous cell cancer (and less commonly adenocarcinoma) | |||
*# '''<span style="color:#ff0000">Alkylating chemotherapy</span>''' | |||
*#* '''Cyclophosphamide''' or ifosfamide | |||
*# '''<span style="color:#ff0000">Analgesic abuse</span>''' | |||
*#* Phenacetin is the most well described causative agent in analgesic nephropathy, others include codeine, acetaminophen, and aspirin. | |||
*#* The number of cases attributed to phenacetin has decreased since phenacetin was replaced by its non-toxigenic metabolite acetaminophen | |||
*#'''<span style="color:#ff0000">Arsenic</span>''' | |||
*#* Exposure can be from drinking water from artesian wells | |||
*#'''<span style="color:#ff0000">History of bladder cancer</span>''' | |||
*#* '''Primary upper urinary tract tumors are uncommon''' | |||
*#**'''Most UTUC occur as secondary tumors that present after NMIBC'''[https://pubmed.ncbi.nlm.nih.gov/11956428/] | |||
*#*'''<span style="color:#ff0000">2-4% patients with bladder cancer will subsequently develop UTUC</span>''' | |||
*#**Interval ranges from 17-170 months | |||
*#**'''Risk factors for subsequent UTUC in patients undergoing cystectomy for bladder cancer[https://pubmed.ncbi.nlm.nih.gov/23083867/]''' | |||
*#***'''Low-grade tumors''' | |||
*#***'''Non–muscle invasive tumors''' | |||
*#***'''N0 status''' | |||
*#***'''Presence of CIS''' | |||
*#***'''Multiple urothelial recurrences''' | |||
*#***'''Multifocal tumors''' | |||
*#***'''History of previous UTUC''' | |||
*#***'''Positive ureteral margin''' | |||
*#***'''Involvement of male prostatic urethra or female urethra''' | |||
*#**** Based on meta-analysis of 27 studies with 13,185 patients (Picozzi et al, 2012) | |||
*#** '''Long-term surveillance of the upper tract is important in bladder cancer patients''' | |||
* '''<span style="color:#ff0000">Unique to UTUC (1):</span>''' | |||
*# '''<span style="color:#ff0000">Aristolochic acid</span>[https://pubmed.ncbi.nlm.nih.gov/23462915/]''' | |||
*#* Found in plants (Aristolochia fangchi and Aristolochia clematitis) and has mutagenic action; the associated mutation is predominant in patients with Balkan endemic nephropathy and Chinese herb nephropathy. These plants are endemic in Balkan countries and grow as weeds in wheat fields. The incidence of Balkan endemic nephropathy is decreasing. | |||
== Histology == | |||
== | === Normal upper tract urothelium === | ||
* '''Bladder is derived from the endoderm; ureter and renal pelvis are derived from the mesoderm''' | |||
* The urothelial lining of the upper urinary tract closely approximates that of the bladder except for the markedly reduced thickness of the muscle layer and the abutting of the urothelium to the renal parenchyma proximally. | |||
* The epithelial layer is continuous from the level of the calyces to the distal ureter. | |||
** It has been suggested that the urothelial layer may even “extend” into the collecting ducts, raising the possibility that collecting duct renal cancers may be closely related to urothelial cancers and perhaps better treated by agents used for urothelial cancers | |||
* '''Renal pelvis and calyces''' | |||
** '''The walls of the calyces and the pelvis''' '''contain''' fibrous connective tissue and 2 layers of '''smooth muscle''' and are lined on their inner surfaces with urothelium | |||
* Ureter | |||
** The 3 muscular layers of the ureter merge with the 3 muscular layers of the bladder | |||
=== Abnormal urothelium === | |||
==== Benign lesions ==== | |||
* '''Papillomas and inverted papillomas''' | |||
** '''Generally considered benign lesions''' | |||
** '''Association with either synchronous or metachronous UTUC''' | |||
*** '''<span style="color:#ff0000">Follow-up for all cases of inverted papilloma should be continued for at least 2 years after initial diagnosis</span>''' | |||
* '''Von Brunn Nests''' | |||
** '''Reactive proliferation, considered a variation of normal urothelium.''' | |||
==== Metaplasia and dysplasia ==== | |||
* '''<span style="color:#ff0000">In a significant proportion of patients, UTUCs progress from hyperplasia to dysplasia to frank CIS</span>''' | |||
==== Urothelial carcinoma ==== | |||
* '''<span style="color:#ff0000">Majority (90%) of upper tract tumours are urothelial carcinoma</span>[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5308053/]''' | |||
** Squamous and adenocarcinomas comprise a small minority. | |||
* '''UTUC are histologically similar to urothelial carcinoma of the bladder, but <span style="color:#ff0000">the relative thinness of the muscle layer of the renal pelvis and ureter may allow earlier penetration of invasive upper tract tumors than is seen in bladder neoplasms.</span>''' | |||
** '''<span style="color:#ff0000">UTUC is more often invasive and poorly differentiated than bladder cancers. However, in pathologically matched cohorts, cancer-specific outcomes are comparable between urothelial tumours of the upper tract and bladder</span>''' | |||
* '''Reported variants of urothelial carcinoma are squamous cell, glandular, sarcomatoid, micropapillary, neuroendocrine, and lymphoepithelial'''. | |||
** Although all of these variants are considered aggressive tumors, after adjustment for the rest of clinicopathologic characteristics, '''<span style="color:#ff0000">variant histology has not been shown to predict poor clinical outcome in UTUC (unlike bladder cancer)</span>''' | |||
==== Non-urothelial carcinoma ==== | |||
* '''<span style="color:#ff0000">Most commonly squamous cell carcinoma and adenocarcinoma</span>''' | |||
===== Squamous ===== | |||
* '''Frequently associated with a condition of chronic inflammation or infection or with analgesic abuse''' | |||
* '''Typically more aggressive at presentation''' | |||
* Occur 6x more frequently in the renal pelvis than in the ureter | |||
===== Adenocarcinoma ===== | |||
* Rare | |||
* '''Typically associated with long-term obstruction''', '''inflammation, or urinary calculi''' | |||
== TNM staging ([https://www.facs.org/quality-programs/cancer/ajcc/cancer-staging/form-supplement AJCC 8th edition]) == | == TNM staging ([https://www.facs.org/quality-programs/cancer/ajcc/cancer-staging/form-supplement AJCC 8th edition]) == | ||
| Line 152: | Line 168: | ||
*** '''Epithelial spreading may occur in both antegrade and retrograde manners.''' | *** '''Epithelial spreading may occur in both antegrade and retrograde manners.''' | ||
**** Antegrade seeding is more common and thought to be the most likely explanation for the high incidence of recurrence in patients in whom a ureteral stump is left in situ after nephrectomy and incomplete ureterectomy | **** Antegrade seeding is more common and thought to be the most likely explanation for the high incidence of recurrence in patients in whom a ureteral stump is left in situ after nephrectomy and incomplete ureterectomy | ||
== Diagnosis and Evaluation of UTUC == | == Diagnosis and Evaluation of UTUC == | ||
| Line 171: | Line 175: | ||
=== AUA === | === AUA === | ||
*[https://pubmed.ncbi.nlm.nih.gov/37096584/ '''2023 AUA Guidelines on Upper Tract Urothelial Carcinoma'''] | *[https://pubmed.ncbi.nlm.nih.gov/37096584/ '''2023 AUA Guidelines on Upper Tract Urothelial Carcinoma'''] | ||
**'''<span style="color:#ff0000">History and Physical Exam (1):</span>'''**#'''<span style="color:#ff0000">Personal and family history</span>''' | **'''<span style="color:#ff0000">History and Physical Exam (1):</span>''' | ||
**#'''<span style="color:#ff0000">Personal and family history</span>''' | |||
**#*'''<span style="color:#ff0000">To identify known hereditary risk factors for familial diseases associated with Lynch Syndrome</span>''' | **#*'''<span style="color:#ff0000">To identify known hereditary risk factors for familial diseases associated with Lynch Syndrome</span>''' | ||
**'''<span style="color:#ff0000"> | **'''<span style="color:#ff0000">Labs (2):</span>''' | ||
**# '''<span style="color:#ff0000">Selective ipsilateral upper tract urine cytology</span>''' | **# '''<span style="color:#ff0000">Selective ipsilateral upper tract urine cytology</span>''' | ||
**#'''<span style="color:#ff0000">Estimated GFR/Serum Cr</span>''' | **#'''<span style="color:#ff0000">Estimated GFR/Serum Cr</span>''' | ||
| Line 187: | Line 192: | ||
***'''Retrograde pyelograms''' | ***'''Retrograde pyelograms''' | ||
=== | === History and Physical Exam === | ||
==== | ==== History ==== | ||
* <span style="color:#ff0000">'''Signs and Symptoms'''</span> | |||
*'''Most common presenting sign is hematuria''' | ** '''Most common presenting sign is hematuria''' | ||
* '''Flank pain is the second most common symptom'''. | ** '''Flank pain is the second most common symptom'''. | ||
** | *** Pain is typically dull and believed to be '''secondary to a gradual onset of obstruction and hydronephrotic distention'''. | ||
* Some patients are asymptomatic at presentation and are diagnosed when an incidental lesion is found on imaging | ***In some patients, pain can be acute and can mimic renal colic, typically due to the passage of clots that acutely obstruct the collecting system. | ||
** Some patients are asymptomatic at presentation and are diagnosed when an incidental lesion is found on imaging | |||
* <span style="color:#ff0000">'''Personal and family history'''</span> | |||
*<span style="color:#ff0000">'''To identify known hereditary risk factors for familial diseases associated with Lynch Syndrome'''</span> | ** <span style="color:#ff0000">'''To identify known hereditary risk factors for familial diseases associated with Lynch Syndrome'''</span> | ||
**'''If positive, referral for genetic counseling should be offered.[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | ***'''If positive, referral for genetic counseling should be offered.[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | ||
***Patients with Lynch Syndrome undergo routine screening due to increased life-long risk for developing associated malignancies, often occurring before 50 years of age[https://pubmed.ncbi.nlm.nih.gov/37096584/] | ****Patients with Lynch Syndrome undergo routine screening due to increased life-long risk for developing associated malignancies, often occurring before 50 years of age[https://pubmed.ncbi.nlm.nih.gov/37096584/] | ||
**'''<span style="color:#ff0000">Lynch syndrome</span>''' | ***'''<span style="color:#ff0000">Lynch syndrome</span>''' | ||
***Familial, autosomal-dominant multi-organ cancer syndrome | ****Familial, autosomal-dominant multi-organ cancer syndrome | ||
****'''Accounts ≈7-20% of UTUC cases in the U.S''' | |||
* | *****Lynch syndrome may increase the possibility of contralateral upper tract involvement, which is an important potential clinical consideration when developing a treatment plan. | ||
***'''Accounts ≈7-20% of UTUC cases in the U.S''' | ****'''See [[Lynch syndrome|Lynch Syndrome Chapter Notes]]''' | ||
****Lynch syndrome may increase the possibility of contralateral upper tract involvement, which is an important potential clinical consideration when developing a treatment plan. | |||
** | |||
** | |||
=== | === Labs === | ||
==== <span style="color:#ff0000">Selective ipsilateral upper tract urine cytology</span> ==== | ==== <span style="color:#ff0000">Selective ipsilateral upper tract urine cytology</span> ==== | ||
*'''Provides supplemental histologic data to tumor biopsies''' | *'''Provides supplemental histologic data to tumor biopsies''' | ||
**'''High-grade cytology in the setting of low-grade biopsy findings indicates the likely presence of higher-risk features (e.g., high-grade tumor) missed on biopsy sampling.''' | **'''High-grade cytology in the setting of low-grade biopsy findings indicates the likely presence of higher-risk features (e.g., high-grade tumor) missed on biopsy sampling.''' | ||
*Reported according to 7 categories (Paris System): | |||
*#Non-diagnostic | |||
*#Negative for high-grade urothelial carcinoma | |||
*#Atypical urothelial cells | |||
*#Suspicious for high-grade urothelial carcinoma | |||
*#High-grade urothelial carcinoma | |||
*#Low-grade urothelial neoplasm | |||
*#Other malignancies | |||
*'''<span style="color:#ff0000">Test characteristics[https://pubmed.ncbi.nlm.nih.gov/27151340/]</span>''' | |||
**'''High specificity (≈90% with selective cytology)''' | |||
**'''Low sensitivity (≈50% with selective cytology)''' | |||
***'''Sensitivity of cytology is directly related to tumor grade''' | |||
*'''<span style="color:#ff0000">Specimen collection considerations</span>''' | *'''<span style="color:#ff0000">Specimen collection considerations</span>''' | ||
**'''<span style="color:#ff0000">Causes of false-positive cytology (2):</span>''' | **'''<span style="color:#ff0000">Causes of false-positive cytology (2):</span>''' | ||
| Line 232: | Line 236: | ||
**#**'''<span style="color:#ff0000">Cytology should be collected prior to any contrast use to avoid artifactual cellular changes from contrast solutions</span>''' | **#**'''<span style="color:#ff0000">Cytology should be collected prior to any contrast use to avoid artifactual cellular changes from contrast solutions</span>''' | ||
**# '''Inflammation from infection or stones''' | **# '''Inflammation from infection or stones''' | ||
**'''<span style="color:#ff0000">Can be obtained either as barbotage (saline irrigation and aspiration) or by saline irrigation with passive collection (washings)</span>''' | **'''<span style="color:#ff0000">Can be obtained as selective vs. voided urinary specimen</span>''' | ||
***'''Preferred over a voided urinary specimen''', due to (3) | ***'''<span style="color:#ff0000">Selective cytology</span>''' | ||
***#Improve cellular yield | ****'''<span style="color:#ff0000">Obtained either as barbotage (saline irrigation and aspiration) or by saline irrigation with passive collection (washings)</span>''' | ||
***#Avoid potential contamination in case of concomitant bladder and/or prostatic urethral disease | *****'''<span style="color:#ff0000">Collecting selective cytology after tumor biopsy can improve the yield of cells for cytologic analysis.</span>''' | ||
***#Avoid theoretical dilution of the specimen from a normal contralateral unit | ****'''Preferred over a voided urinary specimen''', due to (3) | ||
* | ****#Improve cellular yield | ||
****#Avoid potential contamination in case of concomitant bladder and/or prostatic urethral disease | |||
****#Avoid theoretical dilution of the specimen from a normal contralateral unit | |||
**'''In a patient with an upper tract filling defect and an abnormal voided cytology, must be cautious in determining the site of origin of the malignant cells'''. Ureteral catheterization for collection of urine or washings may provide more accurate cytologic results. | |||
*'''In a patient with an upper tract filling defect and an abnormal voided cytology, must be cautious in determining the site of origin of the malignant cells'''. Ureteral catheterization for collection of urine or washings may provide more accurate cytologic results. | |||
==== <span style="color:#ff0000">Assessment of renal function</span> ==== | ==== <span style="color:#ff0000">Assessment of renal function</span> ==== | ||
*Can help with patient counseling, strategizing treatment sequence (operative approach and administration of systemic therapy), and determination of downstream risks of CKD and potential dialysis. | *Can help with patient counseling, strategizing treatment sequence (operative approach and administration of systemic therapy), and determination of downstream risks of CKD and potential dialysis. | ||
* '''Recommended test: serum creatinine (to calculate an eGFR)''' | * '''<span style="color:#ff0000">Recommended test: serum creatinine (to calculate an eGFR)''' | ||
**For more refined evaluation, split function testing such as with differential renal scan or CT volumetric studies may be considered. | **For more refined evaluation, split function testing such as with differential renal scan or CT volumetric studies may be considered. | ||
**The two formulas for monitoring eGFR commonly reported in the contemporary literature at this time are the [https://www.mdcalc.com/calc/76/mdrd-gfr-equation Modification of Diet in Renal Disease] and [https://www.mdcalc.com/calc/3939/ckd-epi-equations-glomerular-filtration-rate-gfr CKD – Epidemiology Collaboration (CKD-EPI)] equations. | **The two formulas for monitoring eGFR commonly reported in the contemporary literature at this time are the [https://www.mdcalc.com/calc/76/mdrd-gfr-equation Modification of Diet in Renal Disease] and [https://www.mdcalc.com/calc/3939/ckd-epi-equations-glomerular-filtration-rate-gfr CKD – Epidemiology Collaboration (CKD-EPI)] equations. | ||
*'''UTUC with associated hydronephrosis''' | *'''<span style="color:#ff0000">UTUC with associated hydronephrosis''' | ||
**'''Implications on assessment of renal function''' | **'''Implications on assessment of renal function''' | ||
*** Caused by tumor obstruction may falsely under-estimate preoperative renal function and alter decision-making around the use of neoadjuvant chemotherapy (NAC). | *** Caused by tumor obstruction may falsely under-estimate preoperative renal function and alter decision-making around the use of neoadjuvant chemotherapy (NAC). | ||
*** Atrophy of the contralateral (unaffected) renal unit may lead to over-estimates of postoperative renal function in the setting of NU since the kidney with lower differential function will remain in situ | *** Atrophy of the contralateral (unaffected) renal unit may lead to over-estimates of postoperative renal function in the setting of NU since the kidney with lower differential function will remain in situ | ||
**'''Renal decompression either by indwelling ureteric stent or a percutaneous nephrostomy tube placed in an uninvolved renal calyx along with oral fluid hydration for 7-14 days before re-checking eGFR will help to establish a more accurate estimation of baseline renal function.''' | **'''Renal decompression either by indwelling ureteric stent or a percutaneous nephrostomy tube placed in an uninvolved renal calyx along with oral fluid hydration for 7-14 days before re-checking eGFR will help to establish a more accurate estimation of baseline renal function.''' | ||
***'''Ureteric stenting is the preferred method of drainage''' | ***'''<span style="color:#ff0000">Ureteric stenting is the preferred method of drainage''' | ||
****Percutaneous nephrostomy tubes in the setting of UTUC increases risk of tract seeding and has worse quality of life | ****Percutaneous nephrostomy tubes in the setting of UTUC increases risk of tract seeding and has worse quality of life | ||
| Line 264: | Line 262: | ||
* Liver is a common site of metastasis | * Liver is a common site of metastasis | ||
=== | === Imaging === | ||
==== | ==== Primary ==== | ||
===== <span style="color:#ff0000">Options</span> ===== | ===== <span style="color:#ff0000">Options[https://pubmed.ncbi.nlm.nih.gov/37096584/ §]</span> ===== | ||
*'''<span style="color:#ff0000">Cross-sectional imaging of the upper tract with contrast including delayed images</span>''' | |||
**'''<span style="color:#ff0000">Preferred modality: multiphase computed tomography (CT) scan with excretory phase imaging of the urothelium</span>''' | |||
***'''<span style="color:#ff0000">Pooled sensitivity of 92%</span>''' | |||
***'''<span style="color:#ff0000">Pooled specificity of 95%</span>''' | |||
**'''<span style="color:#ff0000">If contraindications to contrast-enhanced CT such as chronic kidney disease (CKD) (e.g. eGFR <30[https://medicine.yale.edu/diagnosticradiology/patientcare/policies/nephropathy/]) or untreatable allergy to iodinated contrast medium, use magnetic resonance (MR) urography</span>''' | |||
***'''<span style="color:#ff0000">MRI is less sensitive than CT, similar specificity</span>''' | |||
**'''<span style="color:#ff0000">If contraindications to multiphasic CT and MR urography, use retrograde pyelography in conjunction with non-contrast axial imaging (renal ultrasound) to assess the upper urinary tracts.</span>''' | |||
===== | ====== <span style="color:#ff0000">CT urography</span> ====== | ||
* High sensitivity (100%) and moderate specificity (60%) for upper tract malignant disease | |||
*'''Typical findings suggestive of an upper urinary tract tumor (3):''' | |||
*# '''Radiolucent filling defects''' | |||
*# '''Non-visualization of the collecting system''' | |||
*# '''Obstruction''' | |||
* '''<span style="color:#ff0000">Differential diagnosis of filling defect includes (11): [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7766367/]</span>''' | |||
*# '''<span style="color:#ff0000">Tumour (UTUC, renal cell carcinoma, renal lymphoma, fibroepithelial polyp)</span>''' | |||
*# '''<span style="color:#ff0000">Blood clot</span>''' | |||
*# '''<span style="color:#ff0000">Suburothelial hemorrhage</span>''' | |||
*#'''<span style="color:#ff0000">Stones</span>'''; higher HFU than urothelial carcinoma | |||
*# '''<span style="color:#ff0000">Renal papillary necrosos/sloughed papilla</span>''' | |||
*# '''<span style="color:#ff0000">Hypertrophied papilla</span>''' | |||
*#'''<span style="color:#ff0000">Inflammation</span>''' | |||
*#'''<span style="color:#ff0000">Fungus ball</span>''' | |||
*# '''<span style="color:#ff0000">Tuberculosis</span>''' | |||
*#'''<span style="color:#ff0000">Polyureteritis cystics</span>''' | |||
*#'''<span style="color:#ff0000">Retroperitoneal fibrosis</span>''' | |||
* '''Urothelial cancers are enhancing on arterial/early nephrographic phase, dark/filling defect in urographic phase.''' | |||
*'''Urothelial cancers have more infiltrative features compared to RCC''' | |||
*'''Radiolucent, noncalcified lesions may require additional evaluation by retrograde urography or ureteroscopy, with or without biopsy and cytology''' | |||
* '''<span style="color:#ff0000">Important to evaluate contralateral kidney to assess (2):''' | |||
**'''<span style="color:#ff0000">Possible bilateral disease''' | |||
**'''<span style="color:#ff0000">Functionality of the contralateral kidney''' | |||
[[File:Renal parenchymal phase CT of transitional cell carcinoma.jpg|CT urogram demonstrating filling defect in left renal pelvis. [[commons:File:Renal_parenchymal_phase_CT_of_transitional_cell_carcinoma.jpg|Source]]|center|frame]] | |||
===== | ===== <span style="color:#ff0000">Metastasis</span> ===== | ||
* '''<span style="color:#ff0000">Chest X-Ray</span>''' | |||
* '''<span style="color:#ff0000"> | |||
* '''Bone scan,''' consider in the presence of bone pain, elevated calcium or elevated alkaline phosphatase | * '''Bone scan,''' consider in the presence of bone pain, elevated calcium or elevated alkaline phosphatase | ||
*PET scans[https://pubmed.ncbi.nlm.nih.gov/37096584/] | *PET scans[https://pubmed.ncbi.nlm.nih.gov/37096584/] | ||
**Should not be obtained routinely | **Should not be obtained routinely | ||
**May be selectively considered for patients who are at risk for metastatic recurrence and are not able to have contrast enhanced CT and MRI | **May be selectively considered for patients who are at risk for metastatic recurrence and are not able to have contrast enhanced CT and MRI | ||
*Patients with findings suggestive of metastatic UTUC should be evaluated to define the extent of disease and referred to medical oncology for further management[https://pubmed.ncbi.nlm.nih.gov/37096584/] | *Patients with findings suggestive of metastatic UTUC should be evaluated to define the extent of disease and referred to medical oncology for further management[https://pubmed.ncbi.nlm.nih.gov/37096584/] | ||
=== <span style="color:#ff0000">Other === | === <span style="color:#ff0000">Other === | ||
| Line 375: | Line 375: | ||
*****Bulky bladder tumor involvement where complete resection is not possible | *****Bulky bladder tumor involvement where complete resection is not possible | ||
*****Bulky upper tract disease in which risk assessment is the priority. | *****Bulky upper tract disease in which risk assessment is the priority. | ||
***Some advocate use of ureteral access sheaths to reduce risk of seeding of tumors from bladder to upper tract or from upper tract to the lower tract***The benefits of this approach require further prospective study. | ***Some advocate use of ureteral access sheaths to reduce risk of seeding of tumors from bladder to upper tract or from upper tract to the lower tract | ||
****The benefits of this approach require further prospective study. | |||
** '''In cases of existing ureteral strictures or difficult access to the upper tract, minimize risk of ureteral injury by using gentle dilation techniques such as temporary stenting (pre-stenting) and limit use of aggressive dilation access techniques such as ureteral access sheaths.[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | ** '''In cases of existing ureteral strictures or difficult access to the upper tract, minimize risk of ureteral injury by using gentle dilation techniques such as temporary stenting (pre-stenting) and limit use of aggressive dilation access techniques such as ureteral access sheaths.[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | ||
***Perforation or disruption of the urothelium in patients with UTUC can risk tumor seeding outside the urinary tract. | ***Perforation or disruption of the urothelium in patients with UTUC can risk tumor seeding outside the urinary tract. | ||
| Line 406: | Line 407: | ||
***Identifying the presence of Lynch syndrome-associated and MSI-high cancers also has clinical implications related to therapeutic treatment options, including identified sensitivity of urothelial cancers with mutations in DNA damage repair genes to systemic agents such as immune checkpoint inhibitors and cisplatinum-based chemotherapy | ***Identifying the presence of Lynch syndrome-associated and MSI-high cancers also has clinical implications related to therapeutic treatment options, including identified sensitivity of urothelial cancers with mutations in DNA damage repair genes to systemic agents such as immune checkpoint inhibitors and cisplatinum-based chemotherapy | ||
==== <span style="color:#ff0000"> | ==== <span style="color:#ff0000">Percutaneous biopsy</span> ==== | ||
* '''Systematic review of 288 patients undergoing percutaneous nephroscopic resection of tumour found a tract seeding rate of 0.3%[https://pubmed.ncbi.nlm.nih.gov/22471401/]''' | * Safe and effective technique[https://pubmed.ncbi.nlm.nih.gov/24905868/ §] | ||
*Consider for upper tract urothelial lesions which are not amenable to endoscopic biopsy[https://pubmed.ncbi.nlm.nih.gov/24905868/ §] | |||
*'''Systematic review of 288 patients undergoing percutaneous nephroscopic resection of tumour found a tract seeding rate of 0.3%[https://pubmed.ncbi.nlm.nih.gov/22471401/]''' | |||
==== Urine fluorescence in situ hybridization (FISH) ==== | ==== Urine fluorescence in situ hybridization (FISH) ==== | ||
| Line 416: | Line 419: | ||
*Provide a roadmap for evaluation and possibly planning kidney-preserving strategies | *Provide a roadmap for evaluation and possibly planning kidney-preserving strategies | ||
*Should be considered at initial evaluation with images retained in the patient record | *Should be considered at initial evaluation with images retained in the patient record | ||
=== Special Scenarios === | |||
==== Positive Upper Tract Urinary Cytology ==== | |||
* '''<span style="color:#ff0000">First, repeat the cytology to confirm the findings</span>''' | |||
** '''Any source of inflammation, such as urinary infection or calculus, may produce a false-positive result''' | |||
** A subsequent cytologic abnormality from the contralateral side during follow-up is not rare in cases of true-positive results from early CIS | |||
* '''<span style="color:#ff0000">Next, radiographic evaluation of the upper tracts, usually with CT urography, and a complete bladder evaluation with cystoscopy</span>''' | |||
** '''<span style="color:#ff0000">If the bladder evaluation was</span>''' | |||
*** '''<span style="color:#ff0000">Positive for bladder tumour, treat the bladder and follow the voided urinary cytologies.</span>''' | |||
**** If cytology remains positive despite a negative bladder evaluation or after successful treatment of the bladder, proceed to evaluating extravesical sites. | |||
*** '''<span style="color:#ff0000">Negative for bladder tumour, evaluate extravesical sites.</span>''' | |||
**** '''Evaluation of extravesical sites should include <span style="color:#ff0000">selective cytologies from each upper urinary tract,</span>''' ensuring non-contamination of the specimen from the bladder or urethra, '''as well as resection of a representative <span style="color:#ff0000">specimen of the prostatic urethra in men</span>'''. | |||
***** Selective cytologies should preferably be done, along with ureteroscopy, to allow for direct visualization of the upper urinary tracts. | |||
**** '''In cases of unilateral upper tract cytologic abnormalities''' (with normal cystoscopy, pyelography, and bladder biopsies), '''ureteropyeloscopy is indicated as the next step'''. | |||
***** Ureteropyeloscopy allows for direct visualization of small lesions and is superior to retrograde pyelography in the detection of small tumors. | |||
***** '''Biopsy at the time of ureteropyeloscopy should be attempted, if feasible. A persistently abnormal cytology without any visualized lesions may signify CIS'''. | |||
** | |||
** | |||
* | |||
* | |||
** | |||
** | |||
** | |||
** | |||
** | |||
** | |||
** | |||
** | |||
** | |||
** | |||
* ''' | |||
== Risk-Stratification == | == Risk-Stratification of Localized UTUC == | ||
=== AUA === | === AUA === | ||
| Line 492: | Line 456: | ||
***#**Heterogenous texture on enhanced and even unenhanced CT imaging has been associated with invasive disease | ***#**Heterogenous texture on enhanced and even unenhanced CT imaging has been associated with invasive disease | ||
***#*'''<span style="color:#ff0000">Obstruction of the urinary tract</span>''' | ***#*'''<span style="color:#ff0000">Obstruction of the urinary tract</span>''' | ||
***#*'''<span style="color:#ff0000">Locoregional progression such as suspicious lymphadenopathy</span>''' | ***#*'''<span style="color:#ff0000">Locoregional progression such as suspicious lymphadenopathy</span>''' | ||
***#*'''<span style="color:#ff0000">Presence of metastatic disease</span>''' | ***#*'''<span style="color:#ff0000">Presence of metastatic disease</span>''' | ||
***#'''<span style="color:#ff0000">Endoscopic appearance</span>''' | ***#'''<span style="color:#ff0000">Endoscopic appearance</span>''' | ||
***#*'''<span style="color:#ff0000">Appearance (sessile, papillary, flat/villous)</span>''' | |||
***#*'''<span style="color:#ff0000">Multifocality</span>''' | ***#*'''<span style="color:#ff0000">Multifocality</span>''' | ||
***#* '''<span style="color:#ff0000">Size</span>''' | ***#*'''<span style="color:#ff0000">Size</span>''' | ||
***#**Tumors ≥ 1.5 cm in size are associated with a > 80% risk of invasive disease | ***#**Tumors ≥ 1.5 cm in size are associated with a > 80% risk of invasive disease | ||
***#**Measurement in the pre-surgical setting is not standardized and has not been shown to be independent of other more easily determined clinically identified features such as multifocality, invasion and obstruction. | ***#**Measurement in the pre-surgical setting is not standardized and has not been shown to be independent of other more easily determined clinically identified features such as multifocality, invasion and obstruction. | ||
***#'''<span style="color:#ff0000">Lower tract involvement</span>''' | ***#'''<span style="color:#ff0000">Lower tract involvement</span>''' | ||
***#*'''Pan-urothelial disease as indicated by history of prior cystectomy, concomitant or metachronous lower tract urothelial cancer or contralateral UTUC diagnosis''' | ***#*'''Pan-urothelial disease as indicated by history of prior cystectomy, concomitant or metachronous lower tract urothelial cancer or contralateral UTUC diagnosis''' | ||
=== | == Management == | ||
== | === Non-metastatic disease === | ||
=== <span style="color:#ff0000"> | ==== Options (4) ==== | ||
{| class="wikitable" style="width: 80%; margin: 0 auto;" | |||
|- | |||
| style="width: 40%;" | '''<span style="color:#ff0000">Nephron-sparing (3)</span>''' | |||
| style="width: 40%;" | '''<span style="color:#ff0000">Non Nephron-sparing (1)</span>''' | |||
|- | |||
| | |||
#'''<span style="color:#ff0000">Endoscopic Ablation/Resection</span>''' | |||
## Ureteroscopic | |||
# '''<span style="color:#ff0000">Endoscopic | |||
##Ureteroscopic | |||
## Percutaneous | ## Percutaneous | ||
# '''<span style="color:#ff0000">Intraluminal | # '''<span style="color:#ff0000">Intraluminal Therapy</span>''' | ||
'''Can also be classified as | # '''<span style="color:#ff0000">Segmental Ureterectomy</span>''' | ||
| | |||
#'''<span style="color:#ff0000">Radical nephroureterectomy with bladder cuff excision</span>''' | |||
|} | |||
* Can also be classified as surgical removal (radical nephroureterectomy or segmental ureterectomy) vs. non-surgical removal (endoscopic ablation/resection or intraluminal therapy) | |||
*'''Nephron-sparing approaches are associated with high risk of local recurrence'''; '''patients need to be followed vigilantly for disease progression.''' | |||
=====Endoscopic Ablation/Resection===== | |||
* '''Advantages''' | |||
*# '''Minimally-invasive''' | |||
*# '''Preserves renal function''' | |||
* '''Disadvantages''' | |||
*# '''High risk of recurrence''' | |||
*# '''Risk of disease progression remains''' | |||
*#* '''Due to the suboptimal performance of imaging and biopsy for risk stratification and tumour biology''' | |||
* | |||
* | |||
*''' | |||
* | |||
* | |||
* | |||
*''' | |||
====== Technical considerations ====== | ====== Technical considerations ====== | ||
*'''Approach''' | *'''Approach''' | ||
** '''Retrograde (ureteroscopic) vs. antegrade (percutaneous)''' | ** '''Retrograde (ureteroscopic) vs. antegrade (percutaneous)''' | ||
| Line 668: | Line 519: | ||
***# '''Some portions of the upper urinary tract, such as the lower pole calyces, cannot be reliably reached with working instruments.''' | ***# '''Some portions of the upper urinary tract, such as the lower pole calyces, cannot be reliably reached with working instruments.''' | ||
*** '''Technique''' | *** '''Technique''' | ||
**** | **** Without ureteroscopic resectoscope | ||
**** | *****Debulk tumor by use of either biopsy forceps or a flat wire basket engaged adjacent to the tumor. | ||
******This technique is especially useful for low-grade papillary tumor on a narrow stalk. | |||
*****Treat tumor base with either electrocautery or laser energy sources. | |||
*****Send specimen for pathologic evaluation. | |||
**** With ureteroscopic resectoscope | |||
*****Use resectoscope to remove the tumor. | |||
******Only the intraluminal tumor is resected, and no attempt is made to resect deep (beyond the lamina propria). | |||
**** A ureteral stent is placed for a variable duration to aid with the healing process. | **** A ureteral stent is placed for a variable duration to aid with the healing process. | ||
** '''Antegrade approach''' | ** '''Antegrade approach''' | ||
| Line 684: | Line 540: | ||
***# '''Potential for tumor seeding outside the urinary tract; tract seeding is a possibility but appears to be an uncommon event''' | ***# '''Potential for tumor seeding outside the urinary tract; tract seeding is a possibility but appears to be an uncommon event''' | ||
*** '''Technique''' | *** '''Technique''' | ||
**** '''A nephrostomy tube is left in place.''' This access can be used for second-look follow-up nephroscopy to ensure complete tumor removal. Follow-up (second-look) nephroscopy is performed 4-14 days later to allow adequate healing. The tumor resection site is identified, and any residual tumor is removed. | **** '''A nephrostomy tube is left in place.''' | ||
*****This access can be used for second-look follow-up nephroscopy to ensure complete tumor removal. | |||
****Follow-up (second-look) nephroscopy is performed 4-14 days later to allow adequate healing. | |||
*****The tumor resection site is identified, and any residual tumor is removed. | |||
**** Complications from percutaneous management of tumors are similar to those for benign renal processes and include bleeding, systemic absorption of hypo-osmotic irrigation (with monopolar resection), perforation of the collecting system, and secondary ureteropelvic junction obstruction. | **** Complications from percutaneous management of tumors are similar to those for benign renal processes and include bleeding, systemic absorption of hypo-osmotic irrigation (with monopolar resection), perforation of the collecting system, and secondary ureteropelvic junction obstruction. | ||
*'''Tumor size[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | |||
** '''Tumors < 1.5 cm in size may be optimal for endoscopic ablation given a lower risk of invasive disease.''' | |||
*** Tumors ≥ 1.5 cm in size are associated with a > 80% risk of invasive disease | |||
***'''Larger tumors (≥ 1.5 cm) may be considered for ablation based on the provider’s experience and assessment of the need for kidney sparing surgery.''' | |||
*Energy source[https://pubmed.ncbi.nlm.nih.gov/37096584/] | |||
***Thulium | **Can be performed with laser or electrocautery | ||
***Electrocautery is delivered through a small Bugbee electrode (2 or 3 Fr) | |||
****However, the variable depth of penetration can make its use in the ureter dangerous, and circumferential fulguration should be avoided because of the high risk of stricture formation. | |||
***Thulium, holmium (Ho:YAG), and Neodymium (Nd:YAG) are laser energies that have been used | |||
* Chemoablation[https://pubmed.ncbi.nlm.nih.gov/37096584/] | |||
**May be employed either through retrograde ureteral catheter instillation or percutaneous access with fluoroscopic imaging guidance | |||
*Ureteral access sheath[https://pubmed.ncbi.nlm.nih.gov/37096584/] | |||
**Prior to placement of any ureteral access sheath, the entire ureter should be directly visualized in order to avoid missing any luminal neoplasms, especially in the distal ureter | |||
** Advantages (3): | |||
**#Allows for repeated scope passage up and down the ureter for sampling | |||
**#Means of fluid egress from the upper tract to avoid excess pelvicalyceal hydrostatic pressure from irrigation solutions | |||
**#Lower rate of intravesical recurrence (based on observational study) | |||
====== Outcomes ====== | |||
* '''<span style="color:#ff00ff">Systematic review of endoscopic management of UTUC (2012)</span>''' | |||
** Results: | |||
*** Included 34 studies, 22 on URS and 12 on percutaneous resection | |||
**** All were case series (level of evidence 4), or non-randomized comparative studies (level of evidence 3b) | |||
*** Mean sample size | |||
**** URS: 33 | |||
**** PCN: 24 | |||
**** 3 institutions for URS and 1 for PCN, have published outcomes on cohorts of ≥ 40 patients with > 50 months follow-up, limiting generalizability | |||
*** Estimated 5-yr: | |||
**** Recurrence-free survival: 13 – 54% | |||
**** Renal preservation: 85% | |||
**** Cancer-specific survival: 49-89% | |||
**** OS 57-75% | |||
**** Recurrence-free and cancer-specific survival outcomes worsened with increasing grade | |||
*** [https://pubmed.ncbi.nlm.nih.gov/22471401/ Cutress, Mark L., et al. "Ureteroscopic and percutaneous management of upper tract urothelial carcinoma (UTUC): systematic review." ''BJU international'' 110.5 (2012): 614-628.] | |||
* '''Given high risk of recurrence with endoscopic management, patients should be informed of the need for early second-look and stringent surveillance.''' | |||
======Adjuvant therapy====== | ======Adjuvant therapy====== | ||
* ''' | * Options (2):''' | ||
* '''<span style="color:#ff0000"> | *# Intraluminal/instillation (chemo- or immunotherapy) therapy (see below) | ||
* | *# Brachytherapy of the nephrostomy tract through iridium wire or delivery system | ||
* | |||
*''' | ======Repeat Endoscopic Evaluation[https://pubmed.ncbi.nlm.nih.gov/37096584/]====== | ||
** | *'''<span style="color:#ff0000">Should be performed within 3 months</span>''' | ||
** Systematic review and meta-analysis (2019) | **Proclivity of UTUC to recur and for residual disease to remain after the first ablation | ||
**A 30-day window on either side of this endpoint (i.e., 30 to 90 days) is justified to allow timely identification of recurrences and may be dictated by aspects such as tumor size, visualization, access, treatment efficacy, etc., as clinically indicated | |||
**'''<span style="color:#ff0000">If residual disease identified, repeat endoscopic assessment should occur within 3-month intervals until no evidence of upper tract disease is identified.</span>''' | |||
*'''In patients with LR UTUC with evidence of risk group progression (tumor size, focality, or grade) or when tumor ablation is not feasible,''' further endoscopic-assisted attempts are not recommended. '''surgical resection of all involved sites either by RNU or segmental resection of the ureter should be offered.''' | |||
=====Intraluminal Therapy===== | |||
====== Indications (3): ====== | |||
# '''Adjuvant therapy after endoscopic or organ-sparing therapy''' | |||
#'''Primary treatment for CIS (see Special Scenarios)''' | |||
# '''Primary treatment of low-grade UTUC (UGN-101)''' | |||
====== Adjuvant therapy ====== | |||
*'''Pelvicalyceal or intravesical chemotherapy following ablation of UTUC tumors[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | |||
**Principle of an immediate instillation of intravesical or pyelocaliceal (upper tract) chemotherapy at the time of endoscopic tumor ablation for UTUC is undertaken by extrapolation of the data supporting immediate instillation of intravesical chemotherapy at the time of transurethral resection of a bladder tumor | |||
**Options: thiotepa, mitomycin | |||
**'''Indications''' | |||
*** '''Considered optional''' | |||
** Technique | |||
***Prior to administration, must confirm that there is no perforation of the bladder or upper tract | |||
***Approaches (3) | |||
***#Antegrade perfusion by nephrostomy tube | |||
***#Retrograde perfusion via ureteral catheter | |||
***#Bladder instillation by transurethral catheter with reflux via a double J ureteral stent. | |||
***#*In the third scenario, a cystogram and demonstration of adequate reflux of contrast into the pyelocaliceal system is recommended. | |||
*'''Immunotherapy''' | |||
**'''Pelvicalyceal BCG[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | |||
***'''Indications''' | |||
****'''May be offered to patients with HR favorable UTUC after complete tumor ablation or patients with upper tract carcinoma in situ (CIS).''' | |||
****'''Imperative indications''' | |||
****#'''Solitary kidney status''' | |||
****# '''Bilateral UTUC''' | |||
****#'''Risk of progression to end-stage renal disease''' | |||
***Consists of a 6-week induction course of BCG | |||
* '''Outcomes''' | |||
**'''<span style="color:#ff00ff">Systematic review and meta-analysis (2019)</span>''' | |||
*** Inclusion criteria: studies evaluating patients with upper tract urothelial carcinoma receiving instillation treatment as adjuvant/curative therapy for pTa/pT1 and CIS, respectively. | *** Inclusion criteria: studies evaluating patients with upper tract urothelial carcinoma receiving instillation treatment as adjuvant/curative therapy for pTa/pT1 and CIS, respectively. | ||
*** Studies with ≥10 participants included in quantitative analyses | *** Studies with ≥10 participants included in quantitative analyses | ||
| Line 719: | Line 633: | ||
**** Overall survival: 71% | **** Overall survival: 71% | ||
**** No difference in survival based on approach (antegrade, retrograde, or combined) or drug (MMC vs. BCG) | **** No difference in survival based on approach (antegrade, retrograde, or combined) or drug (MMC vs. BCG) | ||
*** Foerster, Beat, et al. "Endocavitary treatment for upper tract urothelial carcinoma: a meta-analysis of the current literature." ''Urologic Oncology: Seminars and Original Investigations''. Vol. 37. No. 7. Elsevier, 2019. | *** [https://pubmed.ncbi.nlm.nih.gov/30846387/ Foerster, Beat, et al. "Endocavitary treatment for upper tract urothelial carcinoma: a meta-analysis of the current literature." ''Urologic Oncology: Seminars and Original Investigations''. Vol. 37. No. 7. Elsevier, 2019.] | ||
** ''' | * '''Adverse events''' | ||
**''' | **'''Most common complication of intraluminal/instillation therapy is bacterial sepsis''' | ||
*** ''' | |||
*** | ====== <span style="color:#ff0000">Primary treatment for low-grade UTUC</span> ====== | ||
*** | *Effectiveness of intraluminal therapy has been limited by inadequate exposure to urothelium from fluid preparations due to rapid drainage from (2) | ||
*** | **No storage capacity of UTUC (unlike bladder) | ||
*** | **Ureteral and pelvic peristalsis | ||
*** | *Potential solution is to use reverse thermosensitive polymers, which are liquid at room temperature and convert to a gel at body temperature, resulting in increased dwell time | ||
*** | *'''<span style="color:#ff0000">UGN-101</span>''' | ||
*** | **'''UGN-101 = MMC + reverse thermosensitive polymer''' | ||
**''' | ***Also known as Mitogel, Jelmyto | ||
***''' | **'''<span style="color:#ff00ff">OLYMPUS (Lancet Oncology 2020</span>''') | ||
*** | *** Objective: evaluate the safety and activity of UGN-101 to treat primary and recurrent low-grade UTUC. | ||
***''' | *** '''Design: open-label, single-arm, phase 3 trial''' | ||
*** | *** '''Population: 71 patients with primary or recurrent biopsy-proven, low-grade UTUC (involving the renal pelvis or calyces) and ≥1 low-grade lesion above the ureteropelvic junction, measuring 5–15 mm.''' | ||
*** | **** Lesions >15 mm were eligible for endoscopic downsizing before the initiation of treatment. | ||
***#''' | *** Treatment: 6 once-weekly treatments of UGN-101 | ||
* | *** '''Primary outcome: complete response,''' defined as | ||
** | **** Negative endoscopic examination AND | ||
**** Negative cytology at the primary disease evaluation AND | |||
**** Negative for-cause biopsy when done | |||
*** '''Results:''' | |||
**** '''Primary outcome:''' | |||
***** '''≈60% complete response at 3 months''' | |||
****** Among those with complete response, ≈60% maintained complete response at 12 months[https://pubmed.ncbi.nlm.nih.gov/34915741/] | |||
**** '''Adverse events''' | |||
***** Common; 94% had any adverse event | |||
***** 37% had ≥1 serious adverse event | |||
****** '''44% ureteric stenosis[https://pubmed.ncbi.nlm.nih.gov/34915741/]''' | |||
****** 20% renal dysfunction | |||
*** [https://pubmed.ncbi.nlm.nih.gov/32631491/ Kleinmann, Nir, et al.] "Primary chemoablation of low-grade upper tract urothelial carcinoma using UGN-101, a mitomycin-containing reverse thermal gel (OLYMPUS): an open-label, single-arm, phase 3 trial." ''The lancet oncology'' 21.6 (2020): 776-785. | |||
*'''Technique''' | |||
**'''Approaches:''' | |||
***'''Antegrade via percutaneous nephrostomy''' | |||
*** '''Retrograde through a single J open-ended ureteric stent''' | |||
**** '''Suboptimal because the drug often does not reach the renal pelvis''' | |||
*** Both the antegrade and retrograde approach can be dangerous due to possible ureteric obstruction and consecutive pyelovenous influx during instillation/perfusion. | |||
=====Segmental Ureterectomy===== | |||
*'''Reasonable alternative to RNU for well-selected patients''' | |||
====== Options ====== | |||
*'''<span style="color:#ff0000">Segmental ureterectomy with ureteroureterostomy</span>''' | |||
** '''<span style="color:#ff0000">Small, unifocal tumors (typically 1 cm or smaller) tumors isolated to a short segment of the proximal or mid-ureter requiring resection of ≤2 cm or less of ureteral length to allow for primary ureteroureterostomy.</span>''' | |||
***Longer sections of ureteral involvement and resection may require more complex reconstruction techniques when kidney sparing is desired. | |||
*'''<span style="color:#ff0000">Distal ureterectomy with ureteral reimplant</span>''' | |||
**'''<span style="color:#ff0000">Preferred treatment for surgically eligible patients with HR and unfavorable LR cancers endoscopically confirmed as confined to the lower ureter in a functional renal unit</span>''' | |||
***Tumor ablation considered alternative options to the gold-standard of extirpative resection | |||
****Tumor ablation may yield less optimal results and require multiple additional procedures | |||
**Most favorable candidates for distal ureterectomy are patients who | |||
***Have ureteral tumors in the lower third of the ureter | |||
***Sufficiently mobile bladder with capacity to facilitate reimplantation with or without reconfiguration of the bladder to facilitate a tension-free anastomosis (i.e., Boari flap or psoas hitch maneuver). | |||
====== Principles ====== | |||
#'''Patient counseling''' to describe techniques, potential requirements for urinary reconstruction and associated complications including the potential impact on postoperative bladder function. | |||
#'''Preoperative endoscopic assessment''' to evaluate sites of involvement and proximal extent of disease. | |||
#'''Preoperative assessment of bladder capacity''' and function in cases where more extensive reconstruction such as a Boari flap are anticipated to permit a tension free ureterovesical anastomosis or the use of bowel segments. | |||
#'''Intraoperative pathologic assessment''' (i.e., frozen sections) of proximal and distal margins to ensure complete resection with negative margins. | |||
#Reasonable attempts to '''avoid of spillage of urine''' into the surgical field. | |||
# '''Watertight, tension free closure''' to facilitate functional healing and avoid urine leak (of urine potentially contaminated with malignant cells). | |||
====== | ====== Outcomes ====== | ||
*'''<span style="color:# | * '''<span style="color:#ff00ff">Systematic review and meta-analysis comparing segmental resection to radical nephroureterectomy (2020)</span>''' | ||
** | ** Results: | ||
** | *** Included 18 studies comprising 4797 patients, of which 1313 underwent segmental resection | ||
** | *** High risk of bias across all domains analysed, limiting interpretation of comparisons | ||
*** 5-yr: | |||
**** Recurrence-free survival: significantly worse with segmental resection | |||
**** Cancer-specific survival: no significant difference | |||
**** OS: no significant difference | |||
*** Veccia, Alessandro, et al."Segmental ureterectomy for upper tract urothelial carcinoma: a systematic review and meta-analysis of comparative studies." ''Clinical genitourinary cancer'' 18.1 (2020): e10-e20. | |||
* Segmental ureterectomy of the proximal two-thirds of ureter is associated with higher failure rates than for the distal ureter. | |||
==== | ====== Technique ====== | ||
* Risk of wound implantation by tumor is low after open segmental ureterectomy if simple precautions are followed to minimize spillage | |||
*See Segmental Ureterectomy Chapter Notes for technical aspects | |||
*'''When performing NU or distal ureterectomy, the entire distal ureter including the intramural ureteral tunnel and ureteral orifice should be excised, and the urinary tract should be closed in a watertight fashion.''' | |||
**The resultant hiatus in the bladder in the location of the excised ureteral orifice with or without the bladder cuff can be closed formally in a watertight fashion in one or more layers | |||
***A formal BCE with watertight closure of the bladder cuff should be performed to | |||
***#Avoid urinary extravasation from the bladder | |||
***#Facilitate more rapid catheter removal | |||
***#Permit instillation of intravesical adjuvant chemotherapy in the perioperative setting | |||
***Delayed closure by secondary intension in a decompressed bladder without formal bladder closure has also been described. | |||
=====Radical nephroureterectomy with bladder cuff excision===== | |||
===== | ====== Principles[https://pubmed.ncbi.nlm.nih.gov/37096584/] ====== | ||
#'''Complete excision of ipsilateral upper tract urothelium''', including the intramural portion of the ureter and ureteral orifice with negative margins | |||
##Specimen should be removed en bloc whenever technically feasible | |||
# '''Avoidance of urinary spillage,''' such as by early low ligation of the ureter, to minimize the risk of seeding urothelial cancer outside the urinary tract. | |||
====== | ====== Outcomes ====== | ||
*''' | *Largely dependent on clinicopathologic characteristics. | ||
** | *'''<span style="color:#ff00ff">Systematic review and meta-analysis comparing nephron-sparing approach to radical nephroureterectomy (2016)</span>''' | ||
** Primary outcome: cancer-specific survival | |||
** Results | |||
*** Included 22 studies published between 1999 and 2015 | |||
**** No RCTs comparing nephron-sparing approach and nephroureterectomy | |||
*** High risk of bias across all domains analysed, limiting interpretation of comparisons | |||
*** Segemental ureterectomy vs. RNU (10 studies): no significant difference in cancer-specific survival | |||
*** Endoscopic vs. RNU | |||
**** URS vs. RNU (5 studies): no significant difference in cancer-specific survival | |||
***** Grade-based subgroup analyses found decreased cancer-specific survival in patients undergoing URS for high-grade disease | |||
**** Percutaneous resection vs. RNU (2 studies): conflicting findings | |||
** Seisen, Thomas, et al."Oncologic outcomes of kidney-sparing surgery versus radical nephroureterectomy for upper tract urothelial carcinoma: a systematic review by the EAU non-muscle invasive bladder cancer guidelines panel." ''European urology'' 70.6 (2016): 1052-1068. | |||
===== | ====== Technique ====== | ||
* | *See Nephroureterectomy Chapter Notes for technical aspects | ||
*'''Approach[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | *'''Approach[https://pubmed.ncbi.nlm.nih.gov/37096584/]''' | ||
**Open, robotic, and laparoscopic approaches are suitable | **Open, robotic, and laparoscopic approaches are suitable | ||
| Line 771: | Line 747: | ||
**Worse local and metastatic recurrence rates with associated decreased CSS and OS for patients who did not receive complete BCE. | **Worse local and metastatic recurrence rates with associated decreased CSS and OS for patients who did not receive complete BCE. | ||
** Approach | ** Approach | ||
***Extravesical or transvesical | ***Extravesical or transvesical (e.g., midline cystotomy) | ||
***Open, minimally invasive or transurethral endoscopic techniques. | ***Open, minimally invasive or transurethral endoscopic techniques. | ||
****Transurethral endoscopic approaches are associated with higher recurrence rates in the bladder and may limit the ability to utilize post-NU intravesical therapies if the bladder is not fully closed | ****Transurethral endoscopic approaches are associated with higher recurrence rates in the bladder and may limit the ability to utilize post-NU intravesical therapies if the bladder is not fully closed | ||
* | ====== Adverse events ====== | ||
* | *Range from 15% to 50% | ||
==== | * '''30-day mortality risk of 1%''' | ||
====Treatment Selection==== | |||
* '''Based on risk stratification (see above)''' | |||
====== | =====UrologySchool.com Summary===== | ||
*'''<span style="color:#ff0000"> | '''AUA''' | ||
** | *'''<span style="color:#ff0000">If low-risk</span>''' | ||
** | **'''<span style="color:#ff0000">Favorable</span>''' | ||
**''' | ***'''<span style="color:#ff0000">Tumor ablation (preferred, when technically feasible)</span>''' | ||
***''' | ****Observational studies suggest similar cancer-specific survival, similar complication rates, and improved renal function outcomes with endoscopic ablation, compared to nephroureterectomy | ||
***''' | **'''<span style="color:#ff0000">Unfavorable</span>''' | ||
***''' | ***'''<span style="color:#ff0000">Tumor ablation (optional for patients with low-volume tumors or cannot undergo RNU)</span>''' | ||
*** | ***'''<span style="color:#ff0000">Surgical removal (radical nephroureterectomy or segmental ureterectomy)</span>''' | ||
*** | **'''<span style="color:#ff0000">If low-risk and complete endoscopic ablation not feasible, chemoablation (in-situ tissue destruction) with mitomycin containing reverse thermal gel can be a treatment alternative</span>''' | ||
*'''<span style="color:#ff0000">If | *'''<span style="color:#ff0000">If high-risk</span>''' | ||
** | ** '''<span style="color:#ff0000">RNU with complete bladder cuff excision and lymphadenectomy is the standard of care for patients with HR UTUC.</span>''' | ||
**'''<span style="color:#ff0000">Favorable</span>''' | |||
***'''<span style="color:#ff0000">Surgical removal (preferred)</span>''' | |||
***'''<span style="color:#ff0000">Tumor ablation (optional for patients with low-volume tumors or cannot undergo RNU)</span>''' | |||
****'''<span style="color:#ff0000">Select patients who have low-volume tumors or cannot undergo RNU</span>''' | |||
**'''<span style="color:#ff0000">Unfavorable</span>''' | |||
***'''<span style="color:#ff0000">Surgical removal (preferred)</span>''' | |||
**'''<span style="color:#ff0000">For surgically eligible patients with HR and unfavorable LR cancers endoscopically confirmed as confined to the lower ureter in a functional renal unit, distal ureterectomy with ureteral reimplant is the preferred treatment</span>''' | |||
==== Patient counseling[https://pubmed.ncbi.nlm.nih.gov/37096584/] ==== | |||
*'''<span style="color:#ff0000">Discuss and facilitate smoking cessation, if applicable,</span> with patients at the time of diagnosis and treatment.''' | |||
** Risk factors such as smoking are associated with advanced disease stage, recurrence and worse cancer-specific mortality among patients with UTUC, with the highest risk among current smokers. | |||
*'''<span style="color:#ff0000">Provide patients with a description of the short- and long-term risks associated with recommended diagnostic and therapeutic options, including</span>''' | |||
*#'''<span style="color:#ff0000">Need for endoscopic follow-up</span>''' | |||
*#*Urothelial recurrences are common in the management of UTUC, regardless of approach, and mandate long-term surveillance for which patients must be prepared – including the potential need for additional treatments. | |||
*# '''<span style="color:#ff0000">Risks of treatment (3)</span>''' | |||
*##'''<span style="color:#ff0000">Risk of clinically significant strictures with endoscopic management</span>''' | |||
*##*Ablative options can provide local control including durable long-term kidney sparing outcomes but incur additional endoscopic surveillance requirements and associated risks such as stricture and infection | |||
*##*Use of chemoablative treatment with the reverse thermo-hydrogel preparation of mitomycin for pyelocaliceal instillation for LG tumors carries an FDA label warning for ureteral obstruction (>44%), bone marrow suppression, and embryo-fetal toxicity. | |||
*##'''<span style="color:#ff0000">Risk of post-nephroureterectomy CKD or dialysis</span>''' | |||
*##*'''Risk factors for post-operative development of CKD or progression of pre-existing CKD (8):''' | |||
*##*#'''Older age''' | |||
*##*#'''Diabetes mellitus''' | |||
*##*#'''Hypertension''' | |||
*##*#'''Male sex''' | |||
*##*#'''Obesity''' | |||
*##*#'''Tobacco use''' | |||
*##*#'''Larger tumor size''' | |||
*##*#'''Post-operative acute kidney injury.''' | |||
*##*'''Perioperative nephrology consultation can be considered, particularly in patients with pre-existing kidney disease.''' | |||
*##**'''<span style="color:#ff0000">Indications for referral to nephrology (4):</span>''' | |||
*##**# '''<span style="color:#ff0000">eGFR < 45 mL/min/1.73m2</span>''' | |||
*##**#'''<span style="color:#ff0000">Confirmed proteinuria</span>''' | |||
*##**#'''<span style="color:#ff0000">Diabetics with preexisting CKD</span>''' | |||
*##**#'''<span style="color:#ff0000">If eGFR is expected to be < 30 mL/min/1.73m2 after intervention.</span>''' | |||
*##*In patients with pre-existing CKD or a solitary kidney, attempts to preserve renal function can be made, if oncologically feasible and appropriate, with segmental or endoscopic organ-sparing approaches which preferentially are associated with improved postoperative renal function. | |||
*##*In patients with sufficiently poor CKD in which NU could precipitate ESRD, a post operative plan for dialysis in conjunction with nephrology colleagues should be in place preoperatively including plans for dialysis access. Referral to nephrology for detailed evaluation and recommendations for perioperative management is warranted in such cases | |||
*##'''<span style="color:#ff0000">Side effects from neoadjuvant and adjuvant therapies.</span>''' | |||
====Lymph Node Dissection==== | |||
=== | * No RCTs to evaluate the effect of LND on oncologic outcomes in patients undergoing NU or SU | ||
* '''<span style="color:#ff0000">Indications</span>''' | |||
** '''AUA''' | |||
*** '''<span style="color:#ff0000">Recommended (1): HR UTUC</span>''' | |||
**** Sufficient non-randomized evidence to suggest an oncologic benefit to LND at the time of NU for patients with “HR” stratification by guidelines | |||
*** '''<span style="color:#ff0000">Optional (1): LR UTUC</span>''' | |||
**** Limited evidence exists to support a beneficial role for LND at time of NU or ureterectomy among patients with LR UTUC | |||
*'''Template based on tumor collection''' | |||
**'''Pyelocaliceal system: lymph nodes of the ipsilateral great vessel extending from the renal hilum to at least the inferior mesenteric artery.''' | |||
**'''Proximal 2/3 of the ureter: lymph nodes of the ipsilateral great vessel extending from the renal hilum to the aortic bifurcation.''' | |||
**'''Distal 1/3 of the ureter: ipsilateral pelvic LND to include at minimum the obturator and external iliac nodal packets.''' | |||
**Internal and common iliac nodal packets may be removed in the appropriate clinical setting. | |||
**Limited data suggest cranial migration of lymph node metastases to the ipsilateral great vessels such that higher dissection may be considered in the appropriate clinical setting and per clinician judgement | |||
==== Neoadjuvant/Adjuvant Therapy After Complete Excision==== | |||
=====Adjuvant intravesical chemotherapy===== | |||
*'''<span style="color:#ff0000">In patients undergoing RNU or SU (including distal ureterectomy) for UTUC, a single dose of perioperative intravesical chemotherapy should be administered in eligible patients to reduce the risk of bladder recurrence.[https://pubmed.ncbi.nlm.nih.gov/37096584/]</span>''' | |||
**The exact timing of therapy has varied including instilling intravesical chemotherapy at the time of catheter removal (ODMIT-C trial), while other retrospective series reported instillation during surgery or up to 48 hours postoperatively. | |||
***'''<span style="color:#ff00ff">ODMIT-C (2011)</span>''' | |||
*'''<span style="color:#ff0000">In patients undergoing RNU or SU (including distal ureterectomy) for UTUC, a single dose of perioperative intravesical chemotherapy should be administered in eligible patients to reduce the risk of bladder recurrence.[https://pubmed.ncbi.nlm.nih.gov/37096584/]</span>'''**The exact timing of therapy has varied including instilling intravesical chemotherapy at the time of catheter removal (ODMIT-C trial), while other retrospective series reported instillation during surgery or up to 48 hours postoperatively. | **** '''Population: 284 patients with no previous or concurrent history of bladder cancer undergoing nephroureterectomy for suspected UTUC''' | ||
**'''<span style="color:#ff00ff">ODMIT-C (2011)</span>''' | **** '''Randomized to a single postoperative intravesical dose of MMC''' (40 mg in 40 ml saline) '''at the time of urinary catheter removal''' '''vs. standard management''' | ||
*** '''Population: 284 patients with no previous or concurrent history of bladder cancer undergoing nephroureterectomy for suspected UTUC''' | **** '''Results:''' | ||
*** '''Randomized to a single postoperative intravesical dose of MMC''' (40 mg in 40 ml saline) '''at the time of urinary catheter removal''' '''vs. standard management''' | ***** '''Risk of bladder tumour in first year reduced by 11%''' (27% MMC vs. 16% standard treatment) | ||
*** '''Results:''' | **** [https://pubmed.ncbi.nlm.nih.gov/21684068/ O'Brien, Tim, et al.] "Prevention of bladder tumours after nephroureterectomy for primary upper urinary tract urothelial carcinoma: a prospective, multicentre, randomised clinical trial of a single postoperative intravesical dose of mitomycin C (the ODMIT-C Trial)." European urology 60.4 (2011): 703-710. | ||
**** '''Risk of bladder tumour in first year reduced by 11%''' (27% MMC vs. 16% standard treatment) | *** Little data to support one intravesical chemotherapeutic over another. | ||
*** [https://pubmed.ncbi.nlm.nih.gov/21684068/ O'Brien, Tim, et al.] "Prevention of bladder tumours after nephroureterectomy for primary upper urinary tract urothelial carcinoma: a prospective, multicentre, randomised clinical trial of a single postoperative intravesical dose of mitomycin C (the ODMIT-C Trial)." European urology 60.4 (2011): 703-710. | ****Many use gemcitabine over mitomycin due to risks of chemical peritonitis with extravesical extravasation of MMC | ||
** Little data to support one intravesical chemotherapeutic over another. | =====Systemic Therapy===== | ||
***Many use gemcitabine over mitomycin due to risks of chemical peritonitis with extravesical extravasation of MMC | |||
* '''Neoadjuvant''' | * '''Neoadjuvant''' | ||
| Line 857: | Line 841: | ||
** '''Chemotherapy''' | ** '''Chemotherapy''' | ||
*** The use of agents for UTUC has been extrapolated from chemotherapy regimens used in bladder urothelial cancer | *** The use of agents for UTUC has been extrapolated from chemotherapy regimens used in bladder urothelial cancer | ||
*** '''<span style="color:#ff0000">Cisplatin-based neoadjuvant chemotherapy should be offered to patients undergoing RNU or ureterectomy with HR UTUC, particularly in those patients whose post-operative eGFR is expected to be <60 mL/min/1.73m2 or those with other medical comorbidities that would preclude platinum-based chemotherapy in the post-operative setting.[https://pubmed.ncbi.nlm.nih.gov/37096584/]</span>'''****The strongly positive data from these phase II trials, the established high-level evidence seen in bladder cancer trials, the consistent findings from pooled meta-analytic data, and the compelling clinical challenges imposed by post-RNU renal function on cis-platinum eligibility support the standard use of NAC regimens for HR UTUC. | *** '''<span style="color:#ff0000">Cisplatin-based neoadjuvant chemotherapy should be offered to patients undergoing RNU or ureterectomy with HR UTUC, particularly in those patients whose post-operative eGFR is expected to be <60 mL/min/1.73m2 or those with other medical comorbidities that would preclude platinum-based chemotherapy in the post-operative setting.[https://pubmed.ncbi.nlm.nih.gov/37096584/]</span>''' | ||
****The strongly positive data from these phase II trials, the established high-level evidence seen in bladder cancer trials, the consistent findings from pooled meta-analytic data, and the compelling clinical challenges imposed by post-RNU renal function on cis-platinum eligibility support the standard use of NAC regimens for HR UTUC. | |||
****Phase II trial of 30 patients with high-grade UTUC found that 4 cycles of neoadjuvant methotrexate, vinblastine, doxorubicin and cisplatin was associated with a 14% pathological complete response rate.[https://pubmed.ncbi.nlm.nih.gov/31702432/] | ****Phase II trial of 30 patients with high-grade UTUC found that 4 cycles of neoadjuvant methotrexate, vinblastine, doxorubicin and cisplatin was associated with a 14% pathological complete response rate.[https://pubmed.ncbi.nlm.nih.gov/31702432/] | ||
**** 2020 meta-analysis of 14 studies for NAC in UTUC found that the pooled pathologic complete response rate (≤ypT0N0M0) was 11% and pathologic partial response rate (≤ypT1N0M0) was 43%.[https://pubmed.ncbi.nlm.nih.gov/32798146/] | **** 2020 meta-analysis of 14 studies for NAC in UTUC found that the pooled pathologic complete response rate (≤ypT0N0M0) was 11% and pathologic partial response rate (≤ypT1N0M0) was 43%.[https://pubmed.ncbi.nlm.nih.gov/32798146/] | ||
| Line 891: | Line 876: | ||
******Inclusion criteria for both studies were patients with HR urothelial cancer defined as pT3, pT4a, or pN+ for patients who had not received neoadjuvant cisplatin-based chemotherapy and ypT2 to ypT4a or ypN+ for patients who had received neoadjuvant cisplatin | ******Inclusion criteria for both studies were patients with HR urothelial cancer defined as pT3, pT4a, or pN+ for patients who had not received neoadjuvant cisplatin-based chemotherapy and ypT2 to ypT4a or ypN+ for patients who had received neoadjuvant cisplatin | ||
******Adjuvant nivolumab approved for UTUC and urothelial carcinoma of the bladder in patients with advanced disease identified from post-surgical pathology findings | ******Adjuvant nivolumab approved for UTUC and urothelial carcinoma of the bladder in patients with advanced disease identified from post-surgical pathology findings | ||
****Adjuvant platinum-chemotherapy over adjuvant nivolumab is recommended for eligible patients who did not receive NAC. '''Scenarios for use of adjuvant nivolumab include:<span style="color:#ff0000">[https://pubmed.ncbi.nlm.nih.gov/37096584/]</span>''' | ****'''Adjuvant platinum-chemotherapy over adjuvant nivolumab is recommended for eligible patients who did not receive NAC.''' | ||
****'''Scenarios for use of adjuvant nivolumab include:<span style="color:#ff0000">[https://pubmed.ncbi.nlm.nih.gov/37096584/]</span>''' | |||
****#Patients with contraindications to platinum-based chemotherapy (e.g., poor renal function, performance status, sensorineural hearing loss, neuropathy or congestive heart failure, allergy) | ****#Patients with contraindications to platinum-based chemotherapy (e.g., poor renal function, performance status, sensorineural hearing loss, neuropathy or congestive heart failure, allergy) | ||
****#Patients with HR pathology after NAC | ****#Patients with HR pathology after NAC | ||
| Line 898: | Line 884: | ||
**** Radical nephroureterectomy alone provides a high rate of local control; '''adjuvant radiation''' without chemotherapy for high-stage disease '''does not protect against a high rate of distant failure''' | **** Radical nephroureterectomy alone provides a high rate of local control; '''adjuvant radiation''' without chemotherapy for high-stage disease '''does not protect against a high rate of distant failure''' | ||
**** Retrospective studies suggest that there may be a role for combined radiation-chemotherapy regimens in patients with advanced disease with adverse features | **** Retrospective studies suggest that there may be a role for combined radiation-chemotherapy regimens in patients with advanced disease with adverse features | ||
====Special scenarios==== | |||
= | ===== CIS of the Upper Urinary Tracts ===== | ||
* '''In most cases, the diagnosis is one of exclusion wherein there is a persistent positive selective cytology in the absence of any ureteroscopic or radiographic findings.''' | |||
** The diagnosis of CIS of the upper urinary tracts difficult because of the inability to evaluate the urothelium of the upper tracts with adequate tissue samples | |||
* '''Management''' | |||
** '''Not well established''' | |||
** '''<span style="color:#ff0000">Current approaches for presumed upper tract CIS include topical immunotherapy or chemotherapy''' | |||
*** '''Most experience is from use of BCG via a nephrostomy tube for primary treatment of CIS.''' | |||
**** '''<span style="color:#ff00ff">Systematic review and meta-analysis evaluating intraluminal therapy for UTUC (2019)</span>''' | |||
***** Inclusion criteria: studies evaluating patients with upper tract urothelial carcinoma receiving instillation treatment as adjuvant/curative therapy for pTa/pT1 and CIS, respectively. | |||
***** Studies with ≥10 participants included in quantitative analyses | |||
***** Results | |||
****** Included 226 patients from 15 studies of patients that underwent BCG instillation for CIS | |||
****** Recurrence-free survival: 84% | |||
****** Cancer-specific survival: 34% | |||
****** Overall survival: 16% | |||
****** No difference in survival based on approach (antegrade, retrograde, or combined) or drug (MMC vs. BCG) | |||
***** Foerster, Beat, et al. "Endocavitary treatment for upper tract urothelial carcinoma: a meta-analysis of the current literature." ''Urologic Oncology: Seminars and Original Investigations''. Vol. 37. No. 7. Elsevier, 2019. | |||
*** Historically, '''<span style="color:#ff0000">radical nephroureterectomy</span>''' was performed for a unilateral cytologic abnormality of the upper tract to eliminate presumed CIS. This practice '''<span style="color:#ff0000">is not recommended</span>''' in the absence of any histologic, radiographic, or endoscopic finding '''owing to the limitations of cytology alone with false-positive results and the high risk for bilateral disease in the future''' | |||
*** '''Observation is also not appropriate without further evaluation given the repeated abnormal cytologies.''' | |||
* Management of CIS of ureteral margins during radical cystectomy is controversial | |||
* | |||
===== CIS limited to the region within the ureteral orifice ===== | |||
*Topical therapies such as BCG along with refluxing ureteral stenting that has been used for in cases of CIS near the ureterovesical junction or transurethral resection of the transmural portion of the ureter for very distal tumors, as an extension of bladder resection procedures, when tumor is limited to the region inside the ureteral orifice and not beyond the bladder wall, thus anatomically managed as bladder cancer | |||
* | |||
===== Watchful waiting or surveillance ===== | ===== Watchful waiting or surveillance ===== | ||
| Line 975: | Line 916: | ||
*Discussion of treatment related risks including perioperative mortality may lead to a shared decision to proceed with active surveillance (whereby periodic assessments such as imaging or limited endoscopic assessment are performed) or watchful waiting/expectant management, where interventions are limited to palliation or awaiting symptomatic progression – especially in those with very limited life expectancy. | *Discussion of treatment related risks including perioperative mortality may lead to a shared decision to proceed with active surveillance (whereby periodic assessments such as imaging or limited endoscopic assessment are performed) or watchful waiting/expectant management, where interventions are limited to palliation or awaiting symptomatic progression – especially in those with very limited life expectancy. | ||
**In such cases, patients and family should be counseled and prepared for disease-related events such as bleeding, obstruction, infection, and pain with options for palliation that may be limited. | **In such cases, patients and family should be counseled and prepared for disease-related events such as bleeding, obstruction, infection, and pain with options for palliation that may be limited. | ||
=== Advanced disease === | === Advanced disease === | ||
==== Clinical, regional node-positive (N+)==== | ==== Clinical, regional node-positive (N+)==== | ||
| Line 997: | Line 936: | ||
**Formulating alternative care options should be approached with multi-disciplinary input with a focus on realistic goals of care such as providing means of local control for functional preservation (e.g., renal function) and palliation (e.g., bleeding, infection) | **Formulating alternative care options should be approached with multi-disciplinary input with a focus on realistic goals of care such as providing means of local control for functional preservation (e.g., renal function) and palliation (e.g., bleeding, infection) | ||
**Multi-modal approaches include combination of endoscopic management to maintain upper and lower tract function (e.g., stents, nephrostomies, ablation for bleeding and local control) in addition to systemic treatment options if available. Rarely, radiation, angioembolization, or percutaneous ablation for palliation of bleeding can be offered | **Multi-modal approaches include combination of endoscopic management to maintain upper and lower tract function (e.g., stents, nephrostomies, ablation for bleeding and local control) in addition to systemic treatment options if available. Rarely, radiation, angioembolization, or percutaneous ablation for palliation of bleeding can be offered | ||
== Prognosis == | |||
* 5-year overall survival rates: | |||
** Grade | |||
*** 1-2: 40-87% | |||
*** 3-4: 0-33% | |||
** Stage | |||
*** Ta, T1, CIS: 60-90% | |||
*** T2: 43-75% | |||
*** T3: 16-33% | |||
*** T4: 0-5% | |||
*** N+: 0-4% | |||
*** M+: 0% | |||
*'''<span style="color:#ff0000">Prognostic factors</span>''' | |||
**'''<span style="color:#ff0000">Tumour factors</span>''' | |||
**# '''<span style="color:#ff0000">Stage</span>''' | |||
**#* '''<span style="color:#ff0000">Most important prognostic factor</span>''' | |||
**#** '''<span style="color:#ff0000">Non–organ confined disease (>pT2) is the most significant predictor of the development of metastases</span>''' | |||
**# '''<span style="color:#ff0000">Grade</span>''' | |||
**#* '''<span style="color:#ff0000">High-grade tumours are more likely to:</span>''' | |||
**#*# '''<span style="color:#ff0000">Invade</span>''' into the underlying connective tissue, muscle, and surrounding tissues | |||
**#*# '''<span style="color:#ff0000">Be associated with concomitant CIS</span>''' | |||
**#* '''<span style="color:#ff0000">While there is strong correlation between stage and grade, each independently predicts post-operative recurrence</span>''' | |||
**# '''<span style="color:#ff0000">Architecture</span>''' | |||
**#* '''≈85% of renal pelvic tumors are papillary and the remainder sessile''' | |||
**#* '''<span style="color:#ff0000">Papillary tumors seem to have better outcomes than sessile lesions</span>''' | |||
**#** Invasion of the lamina propria or muscle (stage T1 or T2) occurs in 50% of papillary and in >80% of sessile tumors | |||
**#* '''CIS of the upper tract is associated with higher risk for disease progression''' (similar to bladder cancer) and a likelihood of future development of invasive urothelial cancers. | |||
**# '''Size''' | |||
**#* Tumours > 3-4 cm may be associated with worse survival as well as a higher risk of bladder recurrence | |||
**# '''<span style="color:#ff0000">Location</span>''' | |||
**#* '''<span style="color:#ff0000">Renal pelvic tumours are usually more aggressive than ureteral tumours</span>''' | |||
**#** '''<span style="color:#ff0000">50-60% of renal pelvic tumors are invasive''' into either the lamina propria or muscle, </span>'''in''' '''contrast to most bladder tumors, which are usually non-invasive''' | |||
**#** '''<span style="color:#ff0000">55-75% of ureteral tumors are low grade and low stage, but invasion is still more common than bladder tumors</span>''' | |||
**#** The renal parenchyma may be a barrier, slowing distant spread of stage T3 renal pelvis tumors. In contrast, periureteral tumor extension carries a high risk of early tumor dissemination along the periureteral vascular and lymphatic supply. Improved survival of patients with stage T3 renal pelvis tumors versus ureteral tumors has been reported | |||
**#* '''Conflicting results on whether the location of an upper tract tumor affects prognosis''' | |||
**# '''Multifocality''' | |||
**#* Defined as presence of tumor in ≥2 sites within urothelium | |||
**#* Independent predictor of poor clinical outcome | |||
**# '''Tumour necrosis''' | |||
**#* Conflicting evidence on the influence of tumour necrosis on survival | |||
**# '''Lymph node involvement''' | |||
**#* Although lymphadenectomy is seldom performed for clinically node-negative disease, '''pathologic lymph node status is a strong predictor of post-nephroureterectomy recurrence''' | |||
**# LVI | |||
**#* Associated with worse survival in patients without positive nodes; no association in N+ disease | |||
**# Hydronephrosis | |||
**#* Independently associated with advanced disease stage and poor survival | |||
**# Positive surgical margins | |||
**# Previous or concomitant bladder tumours | |||
** '''Patient factors''' | |||
**# Age | |||
**#* Increasing age associated with worse survival | |||
**# Race | |||
**#* Black non-Hispanic race is associated with increased mortality | |||
** '''Surgical factors''' | |||
**# Lack of post-operative mitomycin C instillation | |||
* '''3 particular forms of UTUC,''' 2 associated with environmental exposure ('''aristolochic acid nephropathy''', which includes Balkan and Chinese herbal nephropathy, as well as those seen in arsenic-endemic regions), '''analgesic abuse, and those associated with Lynch syndrome, have an even higher tendency have multiple and bilateral recurrences than do sporadic tumors''' | |||
<h2>Surveillance and Survivorship</h2> | <h2>Surveillance and Survivorship</h2> | ||
===Oncologic Surveillance=== | ===Oncologic Surveillance=== | ||
| Line 1,010: | Line 1,009: | ||
**'''Nephroureterectomy''' | **'''Nephroureterectomy''' | ||
*** '''Intravesical recurrence''' | *** '''Intravesical recurrence''' | ||
****''' | ****<span style="color:#ff0000">'''≈30% patients with UTUC will subsequently develop bladder cancer after nephroureterectomy or nephron-sparing procedures'''</span> | ||
*****'''Most recurrences occur within the first 2 years''' | ***** '''Most recurrences occur within the first 2 years''' | ||
******'''Median time to bladder recurrence 6-12 months''' | |||
******Unclear how long bladder surveillance should continue for after 2 years | ******Unclear how long bladder surveillance should continue for after 2 years | ||
***** '''Given the high incidence of metachronous bladder involvement, routine bladder surveillance should be performed in patients with a history of UTUC''' | |||
***** '''Potential explanations on why bladder cancers following UTUC are more common than UTUC following bladder cancer include:''' | |||
*****# '''Downstream seeding''' | |||
*****# '''Longer exposure time to carcinogens in the bladder''' | |||
*****# '''Greater number of urothelial cells in the bladder that are subject to random carcinogenic events''' | |||
****Risk factors for intravesical recurrence: | ****Risk factors for intravesical recurrence: | ||
****#Male sex | ****#Male sex | ||
| Line 1,040: | Line 1,045: | ||
*****In patients with HG disease, LVI, or tumor multifocality, periodic imaging of the abdomen and pelvis is warranted, particularly for the first 2 years | *****In patients with HG disease, LVI, or tumor multifocality, periodic imaging of the abdomen and pelvis is warranted, particularly for the first 2 years | ||
****Port-site occur very infrequently, usually associated with inadvertent entry into the collecting system. | ****Port-site occur very infrequently, usually associated with inadvertent entry into the collecting system. | ||
****Distant metastases*****Occurred following nephroureterectomy in 16% of patients. | ****Distant metastases | ||
*****Occurred following nephroureterectomy in 16% of patients. | |||
***** Median time to metastases was 13-16 months. | ***** Median time to metastases was 13-16 months. | ||
*****Location of metastases | *****Location of metastases | ||
| Line 1,056: | Line 1,062: | ||
******Non-regional lymph nodes | ******Non-regional lymph nodes | ||
*'''<span style="color:#ff0000">Post-operative evaluation must routinely include evaluation of the:</span>''' | *'''<span style="color:#ff0000">Post-operative evaluation must routinely include evaluation of the:</span>''' | ||
*# '''<span style="color:#ff0000">Bladder, through</span>'''*#*'''<span style="color:#ff0000">Cystoscopy</span>''' | *# '''<span style="color:#ff0000">Bladder, through</span>''' | ||
*#*'''<span style="color:#ff0000">Cystoscopy</span>''' | |||
*# '''<span style="color:#ff0000">Ipsilateral (if organ-sparing therapy was chosen) and contralateral urinary tracts, through</span>''' | *# '''<span style="color:#ff0000">Ipsilateral (if organ-sparing therapy was chosen) and contralateral urinary tracts, through</span>''' | ||
*#*'''<span style="color:#ff0000">Upper tract endoscopy</span>''' | *#*'''<span style="color:#ff0000">Upper tract endoscopy</span>''' | ||
| Line 1,074: | Line 1,081: | ||
====== Surveillance after kidney sparing ====== | ====== Surveillance after kidney sparing ====== | ||
*'''Low-risk patients managed with kidney sparing treatment''' | *'''Low-risk patients managed with kidney sparing treatment''' | ||
**Cystoscopy and upper tract endoscopy within 1-3 months of treatment to confirm successful treatment. | **'''Cystoscopy and upper tract endoscopy within 1-3 months of treatment to confirm successful treatment.''' | ||
**If successful treatment confirmed (no evidence of disease), perform*** Cystoscopy of the bladder once again within the first year after treatment, then at least every 6-9 months for the first 2 years and then at least annually thereafter. | **If successful treatment confirmed (no evidence of disease), perform | ||
*** Upper tract endoscopy at 6 months and 1 year [after treatment]. | ***Cystoscopy of the bladder once again within the first year after treatment, then at least every 6-9 months for the first 2 years and then at least annually thereafter. | ||
****Can be subsequently performed for any symptoms or significant findings on upper tract imaging. | **** Upper tract endoscopy at 6 months and 1 year [after treatment]. | ||
***Upper tract imaging should be performed at least every 6-9 months for first 2 years, then annually up to 5 years. | *****Can be subsequently performed for any symptoms or significant findings on upper tract imaging. | ||
***Surveillance after 5 years in the absence of recurrence should be based on shared decision-making. | ****Upper tract imaging should be performed at least every 6-9 months for first 2 years, then annually up to 5 years. | ||
****Surveillance after 5 years in the absence of recurrence should be based on shared decision-making. | |||
**No distant metastatic evaluation since risk is low with low-risk disease | **No distant metastatic evaluation since risk is low with low-risk disease | ||
*'''High-risk patients managed with kidney sparing treatment''' | *'''High-risk patients managed with kidney sparing treatment''' | ||
**Cystoscopy, upper tract endoscopy, and upper tract urine cytology within 1-3 months of treatment to confirm successful treatment. | **'''Cystoscopy, upper tract endoscopy, and upper tract urine cytology within 1-3 months of treatment to confirm successful treatment.''' | ||
**If successful treatment confirmed (no evidence of disease), perform | **If successful treatment confirmed (no evidence of disease), perform | ||
***Cystoscopy of the bladder and cytology at least every 3-6 months for the first 3 years and then every 6-12 months up to 5 years. | ***Cystoscopy of the bladder and cytology at least every 3-6 months for the first 3 years and then every 6-12 months up to 5 years. | ||
| Line 1,210: | Line 1,218: | ||
</ul> | </ul> | ||
</li> | </li> | ||
</ol><h2> | </ol><h2>References</h2> | ||
<ul> | <ul> | ||
<li>Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, vol 1, chap 58</li><li>[https://pubmed.ncbi.nlm.nih.gov/37096584/ Coleman, Jonathan A., et al. "Diagnosis and Management of Non-Metastatic Upper Tract Urothelial Carcinoma: AUA/SUO Guideline." ''The Journal of Urology'' 209.6 (2023): 1071-1081.] | <li>Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, vol 1, chap 58</li><li>[https://pubmed.ncbi.nlm.nih.gov/37096584/ Coleman, Jonathan A., et al. "Diagnosis and Management of Non-Metastatic Upper Tract Urothelial Carcinoma: AUA/SUO Guideline." ''The Journal of Urology'' 209.6 (2023): 1071-1081.] | ||
</li> | </li> | ||
</ul> | </ul> | ||
Latest revision as of 11:07, 24 June 2024
See 2023 AUA Upper Tract Urothelial Carcinoma Guideline Notes
Includes 2023 AUA Upper Tract Urothelial Carcinoma Guideline Notes
See Video Review of 2023 AUA Guidelines on Upper Tract Urothelial Cancer
Background[edit | edit source]
- UTUC refers to urothelial tumors that originate from the inner lining of the ureter, calyces, or renal pelvis
- Definition of panurothelial disease: disease involving the bladder and 2 extravesical sites
- In males, this could include one or both upper urinary tracts and/or the prostatic urethra
- In females, this could be the bladder and both upper urinary tracts.
- Low incidence and the lack of prospective studies do not permit absolute conclusions about treatment impact and outcomes
Epidemiology[edit | edit source]
- Incidence[1]
- Relatively rare
- US
- Incidence: rate 2/100,000 person-years, 7,000 cases/year
- Tumors of the renal pelvis are slightly more common than ureteral tumors[2]
- Renal pelvis: 1.2/100,000 person-years
- Ureter: 0.8/100,000 person-years
- Ureteral tumours occur more commonly in the lower ureter (70%) than in the upper ureter (25% mid, 5% upper).
- This may be a reflection of downstream implantation.
- Ureteral tumours occur more commonly in the lower ureter (70%) than in the upper ureter (25% mid, 5% upper).
- Tumors of the renal pelvis are slightly more common than ureteral tumors[2]
- Incidence: rate 2/100,000 person-years, 7,000 cases/year
- Higher incidence in Balkan countries (Albania, Bosnia and Herzegovina, Bulgaria, Croatia, Kosovo, Montenegro, North Macedonia, Romania, Serbia, and Slovenia)[3]
- Age
- Peak incidence age 70s and 80s (older than bladder cancer patients)
- Presentation at age <60 should raise concern of hereditary UTUC as part of Lynch syndrome
- Peak incidence age 70s and 80s (older than bladder cancer patients)
- Gender
- M:F 2:1 (unlike bladder which is M:F 4:1)[4]
- Race
- Whites are 2x more likely than Blacks to develop UTUC
Risk Factors[edit | edit source]
Hereditary (1)[edit | edit source]
- Lynch syndrome (hereditary nonpolyposis colorectal carcinoma (HNPCC))
- Compared with non-hereditary cancers, patients are younger (mean age 55 years) and are more likely to be female
Acquired (8)[edit | edit source]
- Risk factors shared with bladder cancer (7)
- Cigarette smoking
- Most important modifiable risk factor for UTUC
- Smoking cessation decreases subsequent risk
- Occupational exposure
- Exposure to aromatic hydrocarbons, especially those used in the chemical, petrol, and plastic industries; other occupations at risk are those with exposure to coal, asphalt, or tar
- Chronic inflammation, infection, or iatrogenesis
- Chronic bacterial infection associated with urinary stones and obstruction has been associated with the development of squamous cell cancer (and less commonly adenocarcinoma)
- Alkylating chemotherapy
- Cyclophosphamide or ifosfamide
- Analgesic abuse
- Phenacetin is the most well described causative agent in analgesic nephropathy, others include codeine, acetaminophen, and aspirin.
- The number of cases attributed to phenacetin has decreased since phenacetin was replaced by its non-toxigenic metabolite acetaminophen
- Arsenic
- Exposure can be from drinking water from artesian wells
- History of bladder cancer
- Primary upper urinary tract tumors are uncommon
- Most UTUC occur as secondary tumors that present after NMIBC[5]
- 2-4% patients with bladder cancer will subsequently develop UTUC
- Interval ranges from 17-170 months
- Risk factors for subsequent UTUC in patients undergoing cystectomy for bladder cancer[6]
- Low-grade tumors
- Non–muscle invasive tumors
- N0 status
- Presence of CIS
- Multiple urothelial recurrences
- Multifocal tumors
- History of previous UTUC
- Positive ureteral margin
- Involvement of male prostatic urethra or female urethra
- Based on meta-analysis of 27 studies with 13,185 patients (Picozzi et al, 2012)
- Long-term surveillance of the upper tract is important in bladder cancer patients
- Primary upper urinary tract tumors are uncommon
- Cigarette smoking
- Unique to UTUC (1):
- Aristolochic acid[7]
- Found in plants (Aristolochia fangchi and Aristolochia clematitis) and has mutagenic action; the associated mutation is predominant in patients with Balkan endemic nephropathy and Chinese herb nephropathy. These plants are endemic in Balkan countries and grow as weeds in wheat fields. The incidence of Balkan endemic nephropathy is decreasing.
- Aristolochic acid[7]
Histology[edit | edit source]
Normal upper tract urothelium[edit | edit source]
- Bladder is derived from the endoderm; ureter and renal pelvis are derived from the mesoderm
- The urothelial lining of the upper urinary tract closely approximates that of the bladder except for the markedly reduced thickness of the muscle layer and the abutting of the urothelium to the renal parenchyma proximally.
- The epithelial layer is continuous from the level of the calyces to the distal ureter.
- It has been suggested that the urothelial layer may even “extend” into the collecting ducts, raising the possibility that collecting duct renal cancers may be closely related to urothelial cancers and perhaps better treated by agents used for urothelial cancers
- Renal pelvis and calyces
- The walls of the calyces and the pelvis contain fibrous connective tissue and 2 layers of smooth muscle and are lined on their inner surfaces with urothelium
- Ureter
- The 3 muscular layers of the ureter merge with the 3 muscular layers of the bladder
Abnormal urothelium[edit | edit source]
Benign lesions[edit | edit source]
- Papillomas and inverted papillomas
- Generally considered benign lesions
- Association with either synchronous or metachronous UTUC
- Follow-up for all cases of inverted papilloma should be continued for at least 2 years after initial diagnosis
- Von Brunn Nests
- Reactive proliferation, considered a variation of normal urothelium.
Metaplasia and dysplasia[edit | edit source]
- In a significant proportion of patients, UTUCs progress from hyperplasia to dysplasia to frank CIS
Urothelial carcinoma[edit | edit source]
- Majority (90%) of upper tract tumours are urothelial carcinoma[8]
- Squamous and adenocarcinomas comprise a small minority.
- UTUC are histologically similar to urothelial carcinoma of the bladder, but the relative thinness of the muscle layer of the renal pelvis and ureter may allow earlier penetration of invasive upper tract tumors than is seen in bladder neoplasms.
- UTUC is more often invasive and poorly differentiated than bladder cancers. However, in pathologically matched cohorts, cancer-specific outcomes are comparable between urothelial tumours of the upper tract and bladder
- Reported variants of urothelial carcinoma are squamous cell, glandular, sarcomatoid, micropapillary, neuroendocrine, and lymphoepithelial.
- Although all of these variants are considered aggressive tumors, after adjustment for the rest of clinicopathologic characteristics, variant histology has not been shown to predict poor clinical outcome in UTUC (unlike bladder cancer)
Non-urothelial carcinoma[edit | edit source]
- Most commonly squamous cell carcinoma and adenocarcinoma
Squamous[edit | edit source]
- Frequently associated with a condition of chronic inflammation or infection or with analgesic abuse
- Typically more aggressive at presentation
- Occur 6x more frequently in the renal pelvis than in the ureter
Adenocarcinoma[edit | edit source]
- Rare
- Typically associated with long-term obstruction, inflammation, or urinary calculi
TNM staging (AJCC 8th edition)[edit | edit source]
- Tstage
- TX: tumour cannot be assessed
- T0: no evidence of tumour
- Ta: non-invasive (confined to epithelial mucosa) papillary carcinoma
- Tis: carcinoma in-situ
- T1: invades lamina propria (subepithelial connective tissue)
- T2: invades muscle
- T3
- Renal pelvis: tumour invades beyond muscularis into peripelvic fat or renal parenchyma
- Ureter: tumour invades beyond muscularis into periureteric fat
- T4: invades adjacent organs or through the kidney into perinephric fat
- Nstage
- NX: regional lymph nodes cannot be assessed
- N0: no regional lymph node metastasis
- N1: metastasis ≤2 cm in greatest dimension, in a single lymph node
- N2: metastasis >2 cm in a single lymph node; or multiple lymph nodes
- Mstage
- MX: distant metastasis cannot be assessed
- M0: no distant metastasis
- M1: distant metastasis
Natural history[edit | edit source]
- Most occurrences are in a single renal unit
- Synchronous bilateral UTUC
- Rare (<2%)
- Risk of bilateral disease and multifocality increases with the presence of CIS
- Metachronous UTUC occurrences are 80% after bladder cancer and 2-6% after contralateral UTUC
- Synchronous bilateral UTUC
- At the time of diagnosis
- ≈25% will present as localized disease
- >50% will present as regionally advanced cancers
- ≈20% will present as distant disease
- UTUC may spread in the same ways as bladder tumors do via direct invasion into the renal parenchyma or surrounding structures, lymphatic or hematogenous invasion, and epithelial spread by seeding or direct extension.
- Lymphatic:
- Lymphatic spread from the upper urinary tract depends on the location of the tumor:
- Renal pelvis and upper ureteral tumors spread initially from hilar to para-aortic and paracaval nodes
- Distal ureteral tumors spread to pelvic nodes
- Risk of lymphatic spread is directly related to the depth of invasion (stage) of the primary tumor
- Lymphatic spread from the upper urinary tract depends on the location of the tumor:
- Hematogenous:
- Most common sites of hematogenous metastases (3):
- Liver
- Lung
- Bone
- Most common sites of hematogenous metastases (3):
- Epithelial:
- Epithelial spreading may occur in both antegrade and retrograde manners.
- Antegrade seeding is more common and thought to be the most likely explanation for the high incidence of recurrence in patients in whom a ureteral stump is left in situ after nephrectomy and incomplete ureterectomy
- Epithelial spreading may occur in both antegrade and retrograde manners.
- Lymphatic:
Diagnosis and Evaluation of UTUC[edit | edit source]
UrologySchool.com Summary[edit | edit source]
AUA[edit | edit source]
- 2023 AUA Guidelines on Upper Tract Urothelial Carcinoma
- History and Physical Exam (1):
- Personal and family history
- To identify known hereditary risk factors for familial diseases associated with Lynch Syndrome
- Personal and family history
- Labs (2):
- Selective ipsilateral upper tract urine cytology
- Estimated GFR/Serum Cr
- Imaging (1):
- CT urogram
- Metastatic staging [not discussed in guidelines]
- Other (3):
- Cystoscopy to assess lower urinary tract
- Upper tract endoscopy and biopsy
- Universal histologic testing of UTUC with additional studies, such as immunohistochemical or microsatellite instability
- Optional (2):
- Urine fluorescence in situ hybridization (FISH)
- Retrograde pyelograms
- History and Physical Exam (1):
History and Physical Exam[edit | edit source]
History[edit | edit source]
- Signs and Symptoms
- Most common presenting sign is hematuria
- Flank pain is the second most common symptom.
- Pain is typically dull and believed to be secondary to a gradual onset of obstruction and hydronephrotic distention.
- In some patients, pain can be acute and can mimic renal colic, typically due to the passage of clots that acutely obstruct the collecting system.
- Some patients are asymptomatic at presentation and are diagnosed when an incidental lesion is found on imaging
- Personal and family history
- To identify known hereditary risk factors for familial diseases associated with Lynch Syndrome
- If positive, referral for genetic counseling should be offered.[9]
- Patients with Lynch Syndrome undergo routine screening due to increased life-long risk for developing associated malignancies, often occurring before 50 years of age[10]
- Lynch syndrome
- Familial, autosomal-dominant multi-organ cancer syndrome
- Accounts ≈7-20% of UTUC cases in the U.S
- Lynch syndrome may increase the possibility of contralateral upper tract involvement, which is an important potential clinical consideration when developing a treatment plan.
- See Lynch Syndrome Chapter Notes
- If positive, referral for genetic counseling should be offered.[9]
- To identify known hereditary risk factors for familial diseases associated with Lynch Syndrome
Labs[edit | edit source]
Selective ipsilateral upper tract urine cytology[edit | edit source]
- Provides supplemental histologic data to tumor biopsies
- High-grade cytology in the setting of low-grade biopsy findings indicates the likely presence of higher-risk features (e.g., high-grade tumor) missed on biopsy sampling.
- Reported according to 7 categories (Paris System):
- Non-diagnostic
- Negative for high-grade urothelial carcinoma
- Atypical urothelial cells
- Suspicious for high-grade urothelial carcinoma
- High-grade urothelial carcinoma
- Low-grade urothelial neoplasm
- Other malignancies
- Test characteristics[11]
- High specificity (≈90% with selective cytology)
- Low sensitivity (≈50% with selective cytology)
- Sensitivity of cytology is directly related to tumor grade
- Specimen collection considerations
- Causes of false-positive cytology (2):
- Contrast agents
- Exposure of urothelial cells to ionic, high-osmolar contrast agents as in retrograde pyelography may worsen cytologic abnormalities.
- Cytology should be collected prior to any contrast use to avoid artifactual cellular changes from contrast solutions
- Exposure of urothelial cells to ionic, high-osmolar contrast agents as in retrograde pyelography may worsen cytologic abnormalities.
- Inflammation from infection or stones
- Contrast agents
- Can be obtained as selective vs. voided urinary specimen
- Selective cytology
- Obtained either as barbotage (saline irrigation and aspiration) or by saline irrigation with passive collection (washings)
- Collecting selective cytology after tumor biopsy can improve the yield of cells for cytologic analysis.
- Preferred over a voided urinary specimen, due to (3)
- Improve cellular yield
- Avoid potential contamination in case of concomitant bladder and/or prostatic urethral disease
- Avoid theoretical dilution of the specimen from a normal contralateral unit
- Obtained either as barbotage (saline irrigation and aspiration) or by saline irrigation with passive collection (washings)
- Selective cytology
- In a patient with an upper tract filling defect and an abnormal voided cytology, must be cautious in determining the site of origin of the malignant cells. Ureteral catheterization for collection of urine or washings may provide more accurate cytologic results.
- Causes of false-positive cytology (2):
Assessment of renal function[edit | edit source]
- Can help with patient counseling, strategizing treatment sequence (operative approach and administration of systemic therapy), and determination of downstream risks of CKD and potential dialysis.
- Recommended test: serum creatinine (to calculate an eGFR)
- For more refined evaluation, split function testing such as with differential renal scan or CT volumetric studies may be considered.
- The two formulas for monitoring eGFR commonly reported in the contemporary literature at this time are the Modification of Diet in Renal Disease and CKD – Epidemiology Collaboration (CKD-EPI) equations.
- UTUC with associated hydronephrosis
- Implications on assessment of renal function
- Caused by tumor obstruction may falsely under-estimate preoperative renal function and alter decision-making around the use of neoadjuvant chemotherapy (NAC).
- Atrophy of the contralateral (unaffected) renal unit may lead to over-estimates of postoperative renal function in the setting of NU since the kidney with lower differential function will remain in situ
- Renal decompression either by indwelling ureteric stent or a percutaneous nephrostomy tube placed in an uninvolved renal calyx along with oral fluid hydration for 7-14 days before re-checking eGFR will help to establish a more accurate estimation of baseline renal function.
- Ureteric stenting is the preferred method of drainage
- Percutaneous nephrostomy tubes in the setting of UTUC increases risk of tract seeding and has worse quality of life
- Ureteric stenting is the preferred method of drainage
- Implications on assessment of renal function
Liver function tests[edit | edit source]
- Liver is a common site of metastasis
Imaging[edit | edit source]
Primary[edit | edit source]
Options§[edit | edit source]
- Cross-sectional imaging of the upper tract with contrast including delayed images
- Preferred modality: multiphase computed tomography (CT) scan with excretory phase imaging of the urothelium
- Pooled sensitivity of 92%
- Pooled specificity of 95%
- If contraindications to contrast-enhanced CT such as chronic kidney disease (CKD) (e.g. eGFR <30[12]) or untreatable allergy to iodinated contrast medium, use magnetic resonance (MR) urography
- MRI is less sensitive than CT, similar specificity
- If contraindications to multiphasic CT and MR urography, use retrograde pyelography in conjunction with non-contrast axial imaging (renal ultrasound) to assess the upper urinary tracts.
- Preferred modality: multiphase computed tomography (CT) scan with excretory phase imaging of the urothelium
CT urography[edit | edit source]
- High sensitivity (100%) and moderate specificity (60%) for upper tract malignant disease
- Typical findings suggestive of an upper urinary tract tumor (3):
- Radiolucent filling defects
- Non-visualization of the collecting system
- Obstruction
- Differential diagnosis of filling defect includes (11): [13]
- Tumour (UTUC, renal cell carcinoma, renal lymphoma, fibroepithelial polyp)
- Blood clot
- Suburothelial hemorrhage
- Stones; higher HFU than urothelial carcinoma
- Renal papillary necrosos/sloughed papilla
- Hypertrophied papilla
- Inflammation
- Fungus ball
- Tuberculosis
- Polyureteritis cystics
- Retroperitoneal fibrosis
- Urothelial cancers are enhancing on arterial/early nephrographic phase, dark/filling defect in urographic phase.
- Urothelial cancers have more infiltrative features compared to RCC
- Radiolucent, noncalcified lesions may require additional evaluation by retrograde urography or ureteroscopy, with or without biopsy and cytology
- Important to evaluate contralateral kidney to assess (2):
- Possible bilateral disease
- Functionality of the contralateral kidney
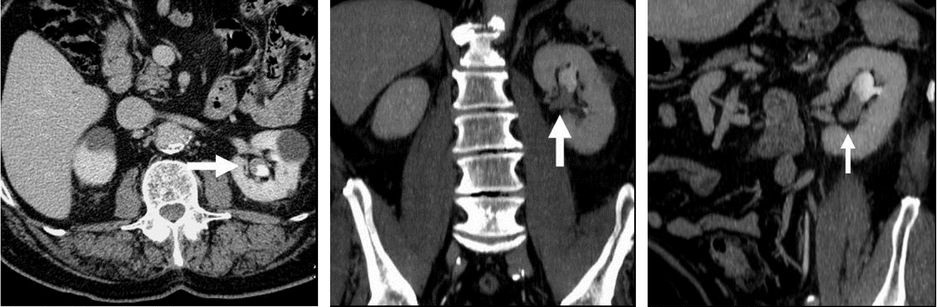
Metastasis[edit | edit source]
- Chest X-Ray
- Bone scan, consider in the presence of bone pain, elevated calcium or elevated alkaline phosphatase
- PET scans[14]
- Should not be obtained routinely
- May be selectively considered for patients who are at risk for metastatic recurrence and are not able to have contrast enhanced CT and MRI
- Patients with findings suggestive of metastatic UTUC should be evaluated to define the extent of disease and referred to medical oncology for further management[15]
Other[edit | edit source]
Cystoscopy[edit | edit source]
- Mandatory because upper urinary tract tumors are often associated with bladder cancers
Upper tract endoscopy +/- biopsy of any identified lesion[edit | edit source]
- Diagnostic ureteroscopy
- Indications for ureteroscopy or percutaneous endoscopy of the upper urinary tract (and when diagnostic and prognostic details are needed)[16]
- Lateralizing hematuria
- Suspicious selective cytology
- Radiographic presence of a mass or urothelial thickening
- Indications for ureteroscopy or percutaneous endoscopy of the upper urinary tract (and when diagnostic and prognostic details are needed)[16]

- URS allows direct visualization of the tumor and biopsy of suspected areas
- Document key descriptive features of UTUC that may guide further diagnostic testing and inform therapeutic interventions as well as provide points of comparison for subsequent ureteroscopic surveillance including:[17]
- Location (ureteral segment, renal pelvis, calyceal sites and lower tract)
- Size
- Number
- Focality
- Appearance (sessile, papillary, flat/villous)
- Quality of visualization
- Can impact the accuracy of endoscopic inspection (e.g., bleeding, difficulty in access, tumor location, artifacts from instrumentation) and should be documented in endoscopic reports.
- See checklist in Guidelines Statement 2,Table 3: Standardized Upper Tract Endoscopy Suggested Reporting Elements
- The urologist’s impression of the tumor grade based on ureteroscopic appearance is likely to be correct in only 70% of cases, suggesting that biopsy is also needed to further define this important aspect of staging
- Biopsy of any identified lesion
- Approaches (2):
- Ureteroscopic biopsy with forceps
- Fluoroscopically guided retrograde brush biopsy
- Mucosal abnormalities may be difficult to biopsy effectively
- Attempted tissue confirmation may be facilitated with the use of brush biopsies or percutaneous image-guided biopsy.
- Approaches (2):
- Biopsy of any identified lesion
- Document key descriptive features of UTUC that may guide further diagnostic testing and inform therapeutic interventions as well as provide points of comparison for subsequent ureteroscopic surveillance including:[17]
- Diagnostic accuracy
- Preoperative determination of the stage of UTUC tumors remains difficult. Therefore, in predicting the tumor stage, a combination of the radiographic studies, the visualized appearance of the tumor, and the tumor grade provides the surgeon with the best estimation for risk stratification.
- Systematic review and meta-analysis evaluating diagnostic accuracy of URS biopsy (2020)
- Included studies comparing URS biopsy to pathology on surgical specimen (radical nephroureterectomy or segmental ureterectomy)
- Results:
- Included 23 studies comprising 2232 patients
- Moderate to high risk of bias accross studies
- Stage-to-stage match
- Positive predictive value for cT1+/muscle-invasive: 94%
- Negative predictive value for cTa-Tis/non-muscle-invasive disease of 60%
- Grade-to-grade match
- High-grade (cHG/pHG): 97%
- Low-grade (cLG/pLG): 66%
- Grade-to-stage match
- Positive predictive value for cHG/muscle-invasive disease: 60%
- Negative predictive value for cLG/non-muscle-invasive disease: 77%
- Overall
- 32% undergrading
- 46% understaging
- A precise correlation with eventual tumor stage is difficult mainly because of technical limitations of use of small biopsy instruments through the narrow channel of the flexible ureteroscope, resulting in the small size and shallow depth of ureteroscopic biopsy specimens. Brush biopsy may be used if cup biopsy forceps fail to obtain adequate tissue.
- Subiela, José Daniel, et al."Diagnostic accuracy of ureteroscopic biopsy in predicting stage and grade at final pathology in upper tract urothelial carcinoma: Systematic review and meta-analysis." European Journal of Surgical Oncology (2020).
- Systematic review and meta-analysis evaluating diagnostic accuracy of URS biopsy (2020)
- Reasonable histologic correlation (78-92%)
- Preoperative determination of the stage of UTUC tumors remains difficult. Therefore, in predicting the tumor stage, a combination of the radiographic studies, the visualized appearance of the tumor, and the tumor grade provides the surgeon with the best estimation for risk stratification.
- In general, CIS of the upper tract is a presumptive diagnosis that is made by the presence of unequivocally positive selective cytology in the absence of any radiographic or endoscopic findings
- Rare situations where endoscopic upper tract evaluation may not be necessary (2)[18]
- Findings would not influence decision-making, such as patients with severe co-morbidities who are ineligible for intervention or request expectant management.
- Other diagnostic means clearly confirm the diagnosis of UTUC and thus histologic tissue confirmation is not clinically required.
- Example would include high-grade (HG) selective cytology or other source of tissue diagnosis, and clear and convincing radiographic findings of upper tract urothelial-based tumor(s) such as an obvious enhancing, urothelial based soft-tissue filling defect on contrast-enhanced imaging with urography.
- Such situations may be particularly relevant in patients with a history of HG urothelial cancer.
- Example would include high-grade (HG) selective cytology or other source of tissue diagnosis, and clear and convincing radiographic findings of upper tract urothelial-based tumor(s) such as an obvious enhancing, urothelial based soft-tissue filling defect on contrast-enhanced imaging with urography.
- If concomitant lower tract tumors (bladder/urethra) are discovered at the time of ureteroscopy, the lower tract tumors should be managed in the same setting as ureteroscopy.[19]
- Consensus on prioritization of procedure sequencing (managing bladder before or after same-setting ureteroscopy) is lacking and heavily scenario-dependent.
- Rationale for managing the bladder first:
- Optimizing visualization within the bladder
- Avoiding back-pressure or back-washing into the upper tract in the case of post-ureteroscopy stenting
- Permitting final confirmation of bladder hemostasis.
- Addressing the upper tract first may be preferred in cases of
- Bulky bladder tumor involvement where complete resection is not possible
- Bulky upper tract disease in which risk assessment is the priority.
- Rationale for managing the bladder first:
- Some advocate use of ureteral access sheaths to reduce risk of seeding of tumors from bladder to upper tract or from upper tract to the lower tract
- The benefits of this approach require further prospective study.
- Consensus on prioritization of procedure sequencing (managing bladder before or after same-setting ureteroscopy) is lacking and heavily scenario-dependent.
- In cases of existing ureteral strictures or difficult access to the upper tract, minimize risk of ureteral injury by using gentle dilation techniques such as temporary stenting (pre-stenting) and limit use of aggressive dilation access techniques such as ureteral access sheaths.[20]
- Perforation or disruption of the urothelium in patients with UTUC can risk tumor seeding outside the urinary tract.
- Recognized perforation or injury events should be documented with immediate cessation of the procedure as soon as safely possible with additional steps to limit sequelae (e.g., stenting, bladder decompression with urethral catheter drainage to limit reflux, nephrostomy tube placement in cases of a completely obstructive ureteral tumor and evidence of contrast extravasation).
- Precautionary measures in cases of difficult ureteral access such as avoiding dilation or placing a stent without performing ureteroscopy and then returning one-two weeks later to repeat the procedure (pre-stenting) can decrease the risk of iatrogenic injury and provide opportunity for a safer and more successful procedure.
- Perforation or disruption of the urothelium in patients with UTUC can risk tumor seeding outside the urinary tract.
- In cases where ureteroscopy cannot be safely performed or is not possible, an attempt at selective upper tract washing or barbotage for cytology may be made and pyeloureterography performed in cases where good quality imaging such as CT or MR urography cannot be obtained.[21]
- When endoscopic examination of the involved upper tract is not possible, findings from selective cytology and retrograde pyelography may provide useful, objective and sufficient information for risk stratification .
- Example scenarios may include washings taken at the time of percutaneous nephrostomy tube placement or during attempted retrograde ureteroscopy that is abandoned for safety concerns.
- When endoscopic examination of the involved upper tract is not possible, findings from selective cytology and retrograde pyelography may provide useful, objective and sufficient information for risk stratification .
- At the time of ureteroscopy for suspected UTUC, ureteroscopic inspection of a radiographically and clinically normal contralateral upper tract should not be performed.[22]
- Endoscopic procedures have risks for patient injury and the potential for tumor seeding in the presence of urothelial cancer. Performing upper tract endoscopy in the setting of a completely normal contralateral upper urinary tract without clinical indication or as a “screening” procedure is unnecessary, placing patients at undue risk and should not be performed
- Technique: Endoscopic Evaluation and Collection of Urine Cytology Specimen
- Summary of Steps
- Cystoscopy is performed and the bladder inspected for concomitant bladder disease.
- The ureteral orifice is identified and inspected for lateralizing hematuria.
- A small-diameter (6.9 or 7.5 Fr) ureteroscope is passed directly into the ureteral orifice, and the distal ureter is inspected before any trauma from a previously placed guidewire or dilation.
- A guidewire is then placed through the ureteroscope and up the ureter to the level of the renal pelvis under fluoroscopic guidance.
- The flexible ureteroscope is used to visualize the remaining urothelium.
- When a lesion or suspicious area is seen, a normal saline washing of the area is performed before biopsy or intervention. If the ureter does not accept the smaller ureteroscope, active dilation of the ureter is necessary.
- Special circumstances include prior urinary diversion and tumor confined to the intramural ureter. With cases of prior urinary diversion, identification of the ureteroenteric anastomosis is difficult and may require antegrade percutaneous passage of a guidewire down the ureter before endoscopy. The wire can be retrieved from the diversion, and the ureteroscope can be passed in a retrograde fashion. The nephrostomy tract does not need to be fully dilated in this setting
- Summary of Steps
- URS allows direct visualization of the tumor and biopsy of suspected areas
- Antegrade endoscopy
- Percutaneous access to the renal pelvis may be required for diagnosis or treatment. In such cases, antegrade urography and ureteroscopy may be useful for tumor resection, biopsy, or simple visualization.
- Tumor cell implantation in the retroperitoneum and along the nephrostomy tube tract has been reported after these procedures
- Percutaneous access to the renal pelvis may be required for diagnosis or treatment. In such cases, antegrade urography and ureteroscopy may be useful for tumor resection, biopsy, or simple visualization.
Universal histologic testing of UTUC with additional studies, such as immunohistochemical (IHC) or microsatellite instability (MSI)[edit | edit source]
- Routine tissue testing provides a more sensitive, first-line means to identify Lynch syndrome-associated features in tumor samples[23]
- Immunohistochemical testing
- Can preliminarily identify the altered proteins associated with Lynch syndrome, and thus help to identify patients who may have the syndrome, who then require confirmation with further genetic (germline) testing
- Widely available
- Microsatellite instability
- Identifying the presence of Lynch syndrome-associated and MSI-high cancers also has clinical implications related to therapeutic treatment options, including identified sensitivity of urothelial cancers with mutations in DNA damage repair genes to systemic agents such as immune checkpoint inhibitors and cisplatinum-based chemotherapy
- Immunohistochemical testing
Percutaneous biopsy[edit | edit source]
- Safe and effective technique§
- Consider for upper tract urothelial lesions which are not amenable to endoscopic biopsy§
- Systematic review of 288 patients undergoing percutaneous nephroscopic resection of tumour found a tract seeding rate of 0.3%[24]
Urine fluorescence in situ hybridization (FISH)[edit | edit source]
- May be considered adjunctively to adjudicate atypical or suspicious cytology results.
Retrograde pyelograms[edit | edit source]
- Provide a roadmap for evaluation and possibly planning kidney-preserving strategies
- Should be considered at initial evaluation with images retained in the patient record
Special Scenarios[edit | edit source]
Positive Upper Tract Urinary Cytology[edit | edit source]
- First, repeat the cytology to confirm the findings
- Any source of inflammation, such as urinary infection or calculus, may produce a false-positive result
- A subsequent cytologic abnormality from the contralateral side during follow-up is not rare in cases of true-positive results from early CIS
- Next, radiographic evaluation of the upper tracts, usually with CT urography, and a complete bladder evaluation with cystoscopy
- If the bladder evaluation was
- Positive for bladder tumour, treat the bladder and follow the voided urinary cytologies.
- If cytology remains positive despite a negative bladder evaluation or after successful treatment of the bladder, proceed to evaluating extravesical sites.
- Negative for bladder tumour, evaluate extravesical sites.
- Evaluation of extravesical sites should include selective cytologies from each upper urinary tract, ensuring non-contamination of the specimen from the bladder or urethra, as well as resection of a representative specimen of the prostatic urethra in men.
- Selective cytologies should preferably be done, along with ureteroscopy, to allow for direct visualization of the upper urinary tracts.
- In cases of unilateral upper tract cytologic abnormalities (with normal cystoscopy, pyelography, and bladder biopsies), ureteropyeloscopy is indicated as the next step.
- Ureteropyeloscopy allows for direct visualization of small lesions and is superior to retrograde pyelography in the detection of small tumors.
- Biopsy at the time of ureteropyeloscopy should be attempted, if feasible. A persistently abnormal cytology without any visualized lesions may signify CIS.
- Evaluation of extravesical sites should include selective cytologies from each upper urinary tract, ensuring non-contamination of the specimen from the bladder or urethra, as well as resection of a representative specimen of the prostatic urethra in men.
- Positive for bladder tumour, treat the bladder and follow the voided urinary cytologies.
- If the bladder evaluation was
Risk-Stratification of Localized UTUC[edit | edit source]
AUA[edit | edit source]
- 2023 AUA Guidelines on Upper Tract Urothelial Carcinoma
- Categorized as high- vs. low-risk of disease progression and pathologic stage ≥T2 disease
- Based on biopsy grade
- Association of high grade tumor on ureteroscopic biopsy with high-stage disease (≥pT2) on final pathology
- Positive predictive value: 60%
- Negative predictive value:77%
- Association of high grade tumor on ureteroscopic biopsy with high-stage disease (≥pT2) on final pathology
- Sub-stratified into favorable vs. unfavorable (see Table 4), based on (4):
- Cytology
- Radiographic appearance
- Multifocality
- Size
- Invasive features
- Heterogenous texture on enhanced and even unenhanced CT imaging has been associated with invasive disease
- Obstruction of the urinary tract
- Locoregional progression such as suspicious lymphadenopathy
- Presence of metastatic disease
- Endoscopic appearance
- Appearance (sessile, papillary, flat/villous)
- Multifocality
- Size
- Tumors ≥ 1.5 cm in size are associated with a > 80% risk of invasive disease
- Measurement in the pre-surgical setting is not standardized and has not been shown to be independent of other more easily determined clinically identified features such as multifocality, invasion and obstruction.
- Lower tract involvement
- Pan-urothelial disease as indicated by history of prior cystectomy, concomitant or metachronous lower tract urothelial cancer or contralateral UTUC diagnosis
- Based on biopsy grade
- Categorized as high- vs. low-risk of disease progression and pathologic stage ≥T2 disease
Management[edit | edit source]
Non-metastatic disease[edit | edit source]
Options (4)[edit | edit source]
| Nephron-sparing (3) | Non Nephron-sparing (1) |
|
|
- Can also be classified as surgical removal (radical nephroureterectomy or segmental ureterectomy) vs. non-surgical removal (endoscopic ablation/resection or intraluminal therapy)
- Nephron-sparing approaches are associated with high risk of local recurrence; patients need to be followed vigilantly for disease progression.
Endoscopic Ablation/Resection[edit | edit source]
- Advantages
- Minimally-invasive
- Preserves renal function
- Disadvantages
- High risk of recurrence
- Risk of disease progression remains
- Due to the suboptimal performance of imaging and biopsy for risk stratification and tumour biology
Technical considerations[edit | edit source]
- Approach
- Retrograde (ureteroscopic) vs. antegrade (percutaneous)
- Choice depends largely on the tumor location and size
- Retrograde preferred when tumor size, number, and access allow complete tumor ablation.
- Percutaneous antegrade tumor ablation preferred for (3):
- Larger tumors
- Tumor difficult to access in a retrograde fashion
- Patients who have undergone prior radical cystectomy or urinary diversion
- In cases with multifocal involvement, combined antegrade and retrograde approaches can be considered
- Choice depends largely on the tumor location and size
- Retrograde approach
- Advantages (2):
- Lower morbidity than percutaneous and open surgical counterparts
- Maintenance of a closed system
- Non-urothelial surfaces are not exposed to the possibility of tumor seeding
- Disadvantages (2):
- Smaller instruments required
- Smaller endoscopes have a smaller field of view and working channel which limits the size of tumor that can be approached in a retrograde fashion. These small instruments limit the accuracy of biopsies, especially with regard to staging
- Some portions of the upper urinary tract, such as the lower pole calyces, cannot be reliably reached with working instruments.
- Smaller instruments required
- Technique
- Without ureteroscopic resectoscope
- Debulk tumor by use of either biopsy forceps or a flat wire basket engaged adjacent to the tumor.
- This technique is especially useful for low-grade papillary tumor on a narrow stalk.
- Treat tumor base with either electrocautery or laser energy sources.
- Send specimen for pathologic evaluation.
- Debulk tumor by use of either biopsy forceps or a flat wire basket engaged adjacent to the tumor.
- With ureteroscopic resectoscope
- Use resectoscope to remove the tumor.
- Only the intraluminal tumor is resected, and no attempt is made to resect deep (beyond the lamina propria).
- Use resectoscope to remove the tumor.
- A ureteral stent is placed for a variable duration to aid with the healing process.
- Without ureteroscopic resectoscope
- Advantages (2):
- Antegrade approach
- Advantages (4):
- Ability to use larger instruments that can remove a large volume of tumor in any portion of the renal collecting system
- Improved tumour staging and grading because deeper biopsy specimens are obtained
- May avoid the limitations of flexible ureteroscopy, especially in complicated calyceal systems or areas difficult to access, such as the lower pole calyx or the upper urinary tract of patients with urinary diversion.
- The established nephrostomy tract can be maintained for immediate postoperative nephroscopy and administration of topical adjuvant therapy
- Disadvantages (4):
- Increased morbidity compared with ureteroscopy
- Risk of nephrostomy tract insertion
- Procedure usually requires inpatient admission
- Potential for tumor seeding outside the urinary tract; tract seeding is a possibility but appears to be an uncommon event
- Technique
- A nephrostomy tube is left in place.
- This access can be used for second-look follow-up nephroscopy to ensure complete tumor removal.
- Follow-up (second-look) nephroscopy is performed 4-14 days later to allow adequate healing.
- The tumor resection site is identified, and any residual tumor is removed.
- Complications from percutaneous management of tumors are similar to those for benign renal processes and include bleeding, systemic absorption of hypo-osmotic irrigation (with monopolar resection), perforation of the collecting system, and secondary ureteropelvic junction obstruction.
- A nephrostomy tube is left in place.
- Advantages (4):
- Retrograde (ureteroscopic) vs. antegrade (percutaneous)
- Tumor size[25]
- Tumors < 1.5 cm in size may be optimal for endoscopic ablation given a lower risk of invasive disease.
- Tumors ≥ 1.5 cm in size are associated with a > 80% risk of invasive disease
- Larger tumors (≥ 1.5 cm) may be considered for ablation based on the provider’s experience and assessment of the need for kidney sparing surgery.
- Tumors < 1.5 cm in size may be optimal for endoscopic ablation given a lower risk of invasive disease.
- Energy source[26]
- Can be performed with laser or electrocautery
- Electrocautery is delivered through a small Bugbee electrode (2 or 3 Fr)
- However, the variable depth of penetration can make its use in the ureter dangerous, and circumferential fulguration should be avoided because of the high risk of stricture formation.
- Thulium, holmium (Ho:YAG), and Neodymium (Nd:YAG) are laser energies that have been used
- Electrocautery is delivered through a small Bugbee electrode (2 or 3 Fr)
- Can be performed with laser or electrocautery
- Chemoablation[27]
- May be employed either through retrograde ureteral catheter instillation or percutaneous access with fluoroscopic imaging guidance
- Ureteral access sheath[28]
- Prior to placement of any ureteral access sheath, the entire ureter should be directly visualized in order to avoid missing any luminal neoplasms, especially in the distal ureter
- Advantages (3):
- Allows for repeated scope passage up and down the ureter for sampling
- Means of fluid egress from the upper tract to avoid excess pelvicalyceal hydrostatic pressure from irrigation solutions
- Lower rate of intravesical recurrence (based on observational study)
Outcomes[edit | edit source]
- Systematic review of endoscopic management of UTUC (2012)
- Results:
- Included 34 studies, 22 on URS and 12 on percutaneous resection
- All were case series (level of evidence 4), or non-randomized comparative studies (level of evidence 3b)
- Mean sample size
- URS: 33
- PCN: 24
- 3 institutions for URS and 1 for PCN, have published outcomes on cohorts of ≥ 40 patients with > 50 months follow-up, limiting generalizability
- Estimated 5-yr:
- Recurrence-free survival: 13 – 54%
- Renal preservation: 85%
- Cancer-specific survival: 49-89%
- OS 57-75%
- Recurrence-free and cancer-specific survival outcomes worsened with increasing grade
- Cutress, Mark L., et al. "Ureteroscopic and percutaneous management of upper tract urothelial carcinoma (UTUC): systematic review." BJU international 110.5 (2012): 614-628.
- Included 34 studies, 22 on URS and 12 on percutaneous resection
- Results:
- Given high risk of recurrence with endoscopic management, patients should be informed of the need for early second-look and stringent surveillance.
Adjuvant therapy[edit | edit source]
- Options (2):
- Intraluminal/instillation (chemo- or immunotherapy) therapy (see below)
- Brachytherapy of the nephrostomy tract through iridium wire or delivery system
Repeat Endoscopic Evaluation[29][edit | edit source]
- Should be performed within 3 months
- Proclivity of UTUC to recur and for residual disease to remain after the first ablation
- A 30-day window on either side of this endpoint (i.e., 30 to 90 days) is justified to allow timely identification of recurrences and may be dictated by aspects such as tumor size, visualization, access, treatment efficacy, etc., as clinically indicated
- If residual disease identified, repeat endoscopic assessment should occur within 3-month intervals until no evidence of upper tract disease is identified.
- In patients with LR UTUC with evidence of risk group progression (tumor size, focality, or grade) or when tumor ablation is not feasible, further endoscopic-assisted attempts are not recommended. surgical resection of all involved sites either by RNU or segmental resection of the ureter should be offered.
Intraluminal Therapy[edit | edit source]
Indications (3):[edit | edit source]
- Adjuvant therapy after endoscopic or organ-sparing therapy
- Primary treatment for CIS (see Special Scenarios)
- Primary treatment of low-grade UTUC (UGN-101)
Adjuvant therapy[edit | edit source]
- Pelvicalyceal or intravesical chemotherapy following ablation of UTUC tumors[30]
- Principle of an immediate instillation of intravesical or pyelocaliceal (upper tract) chemotherapy at the time of endoscopic tumor ablation for UTUC is undertaken by extrapolation of the data supporting immediate instillation of intravesical chemotherapy at the time of transurethral resection of a bladder tumor
- Options: thiotepa, mitomycin
- Indications
- Considered optional
- Technique
- Prior to administration, must confirm that there is no perforation of the bladder or upper tract
- Approaches (3)
- Antegrade perfusion by nephrostomy tube
- Retrograde perfusion via ureteral catheter
- Bladder instillation by transurethral catheter with reflux via a double J ureteral stent.
- In the third scenario, a cystogram and demonstration of adequate reflux of contrast into the pyelocaliceal system is recommended.
- Immunotherapy
- Pelvicalyceal BCG[31]
- Indications
- May be offered to patients with HR favorable UTUC after complete tumor ablation or patients with upper tract carcinoma in situ (CIS).
- Imperative indications
- Solitary kidney status
- Bilateral UTUC
- Risk of progression to end-stage renal disease
- Consists of a 6-week induction course of BCG
- Indications
- Pelvicalyceal BCG[31]
- Outcomes
- Systematic review and meta-analysis (2019)
- Inclusion criteria: studies evaluating patients with upper tract urothelial carcinoma receiving instillation treatment as adjuvant/curative therapy for pTa/pT1 and CIS, respectively.
- Studies with ≥10 participants included in quantitative analyses
- Results
- Included 212 patients from 12 studies of patients that underwent endoscopic laser ablation and instillation therapy for Ta/T1 UTUC
- Recurrence-free survival: 40%
- Similar to recurrence-free survival with observation after nephron-sparing surgery
- Cancer-specific survival: 94%
- Overall survival: 71%
- No difference in survival based on approach (antegrade, retrograde, or combined) or drug (MMC vs. BCG)
- Foerster, Beat, et al. "Endocavitary treatment for upper tract urothelial carcinoma: a meta-analysis of the current literature." Urologic Oncology: Seminars and Original Investigations. Vol. 37. No. 7. Elsevier, 2019.
- Systematic review and meta-analysis (2019)
- Adverse events
- Most common complication of intraluminal/instillation therapy is bacterial sepsis
Primary treatment for low-grade UTUC[edit | edit source]
- Effectiveness of intraluminal therapy has been limited by inadequate exposure to urothelium from fluid preparations due to rapid drainage from (2)
- No storage capacity of UTUC (unlike bladder)
- Ureteral and pelvic peristalsis
- Potential solution is to use reverse thermosensitive polymers, which are liquid at room temperature and convert to a gel at body temperature, resulting in increased dwell time
- UGN-101
- UGN-101 = MMC + reverse thermosensitive polymer
- Also known as Mitogel, Jelmyto
- OLYMPUS (Lancet Oncology 2020)
- Objective: evaluate the safety and activity of UGN-101 to treat primary and recurrent low-grade UTUC.
- Design: open-label, single-arm, phase 3 trial
- Population: 71 patients with primary or recurrent biopsy-proven, low-grade UTUC (involving the renal pelvis or calyces) and ≥1 low-grade lesion above the ureteropelvic junction, measuring 5–15 mm.
- Lesions >15 mm were eligible for endoscopic downsizing before the initiation of treatment.
- Treatment: 6 once-weekly treatments of UGN-101
- Primary outcome: complete response, defined as
- Negative endoscopic examination AND
- Negative cytology at the primary disease evaluation AND
- Negative for-cause biopsy when done
- Results:
- Kleinmann, Nir, et al. "Primary chemoablation of low-grade upper tract urothelial carcinoma using UGN-101, a mitomycin-containing reverse thermal gel (OLYMPUS): an open-label, single-arm, phase 3 trial." The lancet oncology 21.6 (2020): 776-785.
- UGN-101 = MMC + reverse thermosensitive polymer
- Technique
- Approaches:
- Antegrade via percutaneous nephrostomy
- Retrograde through a single J open-ended ureteric stent
- Suboptimal because the drug often does not reach the renal pelvis
- Both the antegrade and retrograde approach can be dangerous due to possible ureteric obstruction and consecutive pyelovenous influx during instillation/perfusion.
- Approaches:
Segmental Ureterectomy[edit | edit source]
- Reasonable alternative to RNU for well-selected patients
Options[edit | edit source]
- Segmental ureterectomy with ureteroureterostomy
- Small, unifocal tumors (typically 1 cm or smaller) tumors isolated to a short segment of the proximal or mid-ureter requiring resection of ≤2 cm or less of ureteral length to allow for primary ureteroureterostomy.
- Longer sections of ureteral involvement and resection may require more complex reconstruction techniques when kidney sparing is desired.
- Small, unifocal tumors (typically 1 cm or smaller) tumors isolated to a short segment of the proximal or mid-ureter requiring resection of ≤2 cm or less of ureteral length to allow for primary ureteroureterostomy.
- Distal ureterectomy with ureteral reimplant
- Preferred treatment for surgically eligible patients with HR and unfavorable LR cancers endoscopically confirmed as confined to the lower ureter in a functional renal unit
- Tumor ablation considered alternative options to the gold-standard of extirpative resection
- Tumor ablation may yield less optimal results and require multiple additional procedures
- Tumor ablation considered alternative options to the gold-standard of extirpative resection
- Most favorable candidates for distal ureterectomy are patients who
- Have ureteral tumors in the lower third of the ureter
- Sufficiently mobile bladder with capacity to facilitate reimplantation with or without reconfiguration of the bladder to facilitate a tension-free anastomosis (i.e., Boari flap or psoas hitch maneuver).
- Preferred treatment for surgically eligible patients with HR and unfavorable LR cancers endoscopically confirmed as confined to the lower ureter in a functional renal unit
Principles[edit | edit source]
- Patient counseling to describe techniques, potential requirements for urinary reconstruction and associated complications including the potential impact on postoperative bladder function.
- Preoperative endoscopic assessment to evaluate sites of involvement and proximal extent of disease.
- Preoperative assessment of bladder capacity and function in cases where more extensive reconstruction such as a Boari flap are anticipated to permit a tension free ureterovesical anastomosis or the use of bowel segments.
- Intraoperative pathologic assessment (i.e., frozen sections) of proximal and distal margins to ensure complete resection with negative margins.
- Reasonable attempts to avoid of spillage of urine into the surgical field.
- Watertight, tension free closure to facilitate functional healing and avoid urine leak (of urine potentially contaminated with malignant cells).
Outcomes[edit | edit source]
- Systematic review and meta-analysis comparing segmental resection to radical nephroureterectomy (2020)
- Results:
- Included 18 studies comprising 4797 patients, of which 1313 underwent segmental resection
- High risk of bias across all domains analysed, limiting interpretation of comparisons
- 5-yr:
- Recurrence-free survival: significantly worse with segmental resection
- Cancer-specific survival: no significant difference
- OS: no significant difference
- Veccia, Alessandro, et al."Segmental ureterectomy for upper tract urothelial carcinoma: a systematic review and meta-analysis of comparative studies." Clinical genitourinary cancer 18.1 (2020): e10-e20.
- Results:
- Segmental ureterectomy of the proximal two-thirds of ureter is associated with higher failure rates than for the distal ureter.
Technique[edit | edit source]
- Risk of wound implantation by tumor is low after open segmental ureterectomy if simple precautions are followed to minimize spillage
- See Segmental Ureterectomy Chapter Notes for technical aspects
- When performing NU or distal ureterectomy, the entire distal ureter including the intramural ureteral tunnel and ureteral orifice should be excised, and the urinary tract should be closed in a watertight fashion.
- The resultant hiatus in the bladder in the location of the excised ureteral orifice with or without the bladder cuff can be closed formally in a watertight fashion in one or more layers
- A formal BCE with watertight closure of the bladder cuff should be performed to
- Avoid urinary extravasation from the bladder
- Facilitate more rapid catheter removal
- Permit instillation of intravesical adjuvant chemotherapy in the perioperative setting
- Delayed closure by secondary intension in a decompressed bladder without formal bladder closure has also been described.
- A formal BCE with watertight closure of the bladder cuff should be performed to
- The resultant hiatus in the bladder in the location of the excised ureteral orifice with or without the bladder cuff can be closed formally in a watertight fashion in one or more layers
Radical nephroureterectomy with bladder cuff excision[edit | edit source]
Principles[34][edit | edit source]
- Complete excision of ipsilateral upper tract urothelium, including the intramural portion of the ureter and ureteral orifice with negative margins
- Specimen should be removed en bloc whenever technically feasible
- Avoidance of urinary spillage, such as by early low ligation of the ureter, to minimize the risk of seeding urothelial cancer outside the urinary tract.
Outcomes[edit | edit source]
- Largely dependent on clinicopathologic characteristics.
- Systematic review and meta-analysis comparing nephron-sparing approach to radical nephroureterectomy (2016)
- Primary outcome: cancer-specific survival
- Results
- Included 22 studies published between 1999 and 2015
- No RCTs comparing nephron-sparing approach and nephroureterectomy
- High risk of bias across all domains analysed, limiting interpretation of comparisons
- Segemental ureterectomy vs. RNU (10 studies): no significant difference in cancer-specific survival
- Endoscopic vs. RNU
- URS vs. RNU (5 studies): no significant difference in cancer-specific survival
- Grade-based subgroup analyses found decreased cancer-specific survival in patients undergoing URS for high-grade disease
- Percutaneous resection vs. RNU (2 studies): conflicting findings
- URS vs. RNU (5 studies): no significant difference in cancer-specific survival
- Included 22 studies published between 1999 and 2015
- Seisen, Thomas, et al."Oncologic outcomes of kidney-sparing surgery versus radical nephroureterectomy for upper tract urothelial carcinoma: a systematic review by the EAU non-muscle invasive bladder cancer guidelines panel." European urology 70.6 (2016): 1052-1068.
Technique[edit | edit source]
- See Nephroureterectomy Chapter Notes for technical aspects
- Approach[35]
- Open, robotic, and laparoscopic approaches are suitable
- Minimally invasive approaches were associated with favorable perioperative outcomes including shorter length of stay and fewer complications, and, therefore, are favored for most patients when principles of RNU can be maintained
- Consider open surgical approaches for large, bulky UTUC with clinical evidence for direct invasion to adjacent structures
- Open, robotic, and laparoscopic approaches are suitable
- Bladder cuff excision[36]
- Worse local and metastatic recurrence rates with associated decreased CSS and OS for patients who did not receive complete BCE.
- Approach
- Extravesical or transvesical (e.g., midline cystotomy)
- Open, minimally invasive or transurethral endoscopic techniques.
- Transurethral endoscopic approaches are associated with higher recurrence rates in the bladder and may limit the ability to utilize post-NU intravesical therapies if the bladder is not fully closed
Adverse events[edit | edit source]
- Range from 15% to 50%
- 30-day mortality risk of 1%
Treatment Selection[edit | edit source]
- Based on risk stratification (see above)
UrologySchool.com Summary[edit | edit source]
AUA
- If low-risk
- Favorable
- Tumor ablation (preferred, when technically feasible)
- Observational studies suggest similar cancer-specific survival, similar complication rates, and improved renal function outcomes with endoscopic ablation, compared to nephroureterectomy
- Tumor ablation (preferred, when technically feasible)
- Unfavorable
- Tumor ablation (optional for patients with low-volume tumors or cannot undergo RNU)
- Surgical removal (radical nephroureterectomy or segmental ureterectomy)
- If low-risk and complete endoscopic ablation not feasible, chemoablation (in-situ tissue destruction) with mitomycin containing reverse thermal gel can be a treatment alternative
- Favorable
- If high-risk
- RNU with complete bladder cuff excision and lymphadenectomy is the standard of care for patients with HR UTUC.
- Favorable
- Surgical removal (preferred)
- Tumor ablation (optional for patients with low-volume tumors or cannot undergo RNU)
- Select patients who have low-volume tumors or cannot undergo RNU
- Unfavorable
- Surgical removal (preferred)
- For surgically eligible patients with HR and unfavorable LR cancers endoscopically confirmed as confined to the lower ureter in a functional renal unit, distal ureterectomy with ureteral reimplant is the preferred treatment
Patient counseling[37][edit | edit source]
- Discuss and facilitate smoking cessation, if applicable, with patients at the time of diagnosis and treatment.
- Risk factors such as smoking are associated with advanced disease stage, recurrence and worse cancer-specific mortality among patients with UTUC, with the highest risk among current smokers.
- Provide patients with a description of the short- and long-term risks associated with recommended diagnostic and therapeutic options, including
- Need for endoscopic follow-up
- Urothelial recurrences are common in the management of UTUC, regardless of approach, and mandate long-term surveillance for which patients must be prepared – including the potential need for additional treatments.
- Risks of treatment (3)
- Risk of clinically significant strictures with endoscopic management
- Ablative options can provide local control including durable long-term kidney sparing outcomes but incur additional endoscopic surveillance requirements and associated risks such as stricture and infection
- Use of chemoablative treatment with the reverse thermo-hydrogel preparation of mitomycin for pyelocaliceal instillation for LG tumors carries an FDA label warning for ureteral obstruction (>44%), bone marrow suppression, and embryo-fetal toxicity.
- Risk of post-nephroureterectomy CKD or dialysis
- Risk factors for post-operative development of CKD or progression of pre-existing CKD (8):
- Older age
- Diabetes mellitus
- Hypertension
- Male sex
- Obesity
- Tobacco use
- Larger tumor size
- Post-operative acute kidney injury.
- Perioperative nephrology consultation can be considered, particularly in patients with pre-existing kidney disease.
- Indications for referral to nephrology (4):
- eGFR < 45 mL/min/1.73m2
- Confirmed proteinuria
- Diabetics with preexisting CKD
- If eGFR is expected to be < 30 mL/min/1.73m2 after intervention.
- Indications for referral to nephrology (4):
- In patients with pre-existing CKD or a solitary kidney, attempts to preserve renal function can be made, if oncologically feasible and appropriate, with segmental or endoscopic organ-sparing approaches which preferentially are associated with improved postoperative renal function.
- In patients with sufficiently poor CKD in which NU could precipitate ESRD, a post operative plan for dialysis in conjunction with nephrology colleagues should be in place preoperatively including plans for dialysis access. Referral to nephrology for detailed evaluation and recommendations for perioperative management is warranted in such cases
- Risk factors for post-operative development of CKD or progression of pre-existing CKD (8):
- Side effects from neoadjuvant and adjuvant therapies.
- Risk of clinically significant strictures with endoscopic management
- Need for endoscopic follow-up
Lymph Node Dissection[edit | edit source]
- No RCTs to evaluate the effect of LND on oncologic outcomes in patients undergoing NU or SU
- Indications
- AUA
- Recommended (1): HR UTUC
- Sufficient non-randomized evidence to suggest an oncologic benefit to LND at the time of NU for patients with “HR” stratification by guidelines
- Optional (1): LR UTUC
- Limited evidence exists to support a beneficial role for LND at time of NU or ureterectomy among patients with LR UTUC
- Recommended (1): HR UTUC
- AUA
- Template based on tumor collection
- Pyelocaliceal system: lymph nodes of the ipsilateral great vessel extending from the renal hilum to at least the inferior mesenteric artery.
- Proximal 2/3 of the ureter: lymph nodes of the ipsilateral great vessel extending from the renal hilum to the aortic bifurcation.
- Distal 1/3 of the ureter: ipsilateral pelvic LND to include at minimum the obturator and external iliac nodal packets.
- Internal and common iliac nodal packets may be removed in the appropriate clinical setting.
- Limited data suggest cranial migration of lymph node metastases to the ipsilateral great vessels such that higher dissection may be considered in the appropriate clinical setting and per clinician judgement
Neoadjuvant/Adjuvant Therapy After Complete Excision[edit | edit source]
Adjuvant intravesical chemotherapy[edit | edit source]
- In patients undergoing RNU or SU (including distal ureterectomy) for UTUC, a single dose of perioperative intravesical chemotherapy should be administered in eligible patients to reduce the risk of bladder recurrence.[38]
- The exact timing of therapy has varied including instilling intravesical chemotherapy at the time of catheter removal (ODMIT-C trial), while other retrospective series reported instillation during surgery or up to 48 hours postoperatively.
- ODMIT-C (2011)
- Population: 284 patients with no previous or concurrent history of bladder cancer undergoing nephroureterectomy for suspected UTUC
- Randomized to a single postoperative intravesical dose of MMC (40 mg in 40 ml saline) at the time of urinary catheter removal vs. standard management
- Results:
- Risk of bladder tumour in first year reduced by 11% (27% MMC vs. 16% standard treatment)
- O'Brien, Tim, et al. "Prevention of bladder tumours after nephroureterectomy for primary upper urinary tract urothelial carcinoma: a prospective, multicentre, randomised clinical trial of a single postoperative intravesical dose of mitomycin C (the ODMIT-C Trial)." European urology 60.4 (2011): 703-710.
- Little data to support one intravesical chemotherapeutic over another.
- Many use gemcitabine over mitomycin due to risks of chemical peritonitis with extravesical extravasation of MMC
- ODMIT-C (2011)
- The exact timing of therapy has varied including instilling intravesical chemotherapy at the time of catheter removal (ODMIT-C trial), while other retrospective series reported instillation during surgery or up to 48 hours postoperatively.
Systemic Therapy[edit | edit source]
- Neoadjuvant
- No randomized trials evaluating benefit of neoadjuvant therapy for UTUC.
- Chemotherapy
- The use of agents for UTUC has been extrapolated from chemotherapy regimens used in bladder urothelial cancer
- Cisplatin-based neoadjuvant chemotherapy should be offered to patients undergoing RNU or ureterectomy with HR UTUC, particularly in those patients whose post-operative eGFR is expected to be <60 mL/min/1.73m2 or those with other medical comorbidities that would preclude platinum-based chemotherapy in the post-operative setting.[39]
- The strongly positive data from these phase II trials, the established high-level evidence seen in bladder cancer trials, the consistent findings from pooled meta-analytic data, and the compelling clinical challenges imposed by post-RNU renal function on cis-platinum eligibility support the standard use of NAC regimens for HR UTUC.
- Phase II trial of 30 patients with high-grade UTUC found that 4 cycles of neoadjuvant methotrexate, vinblastine, doxorubicin and cisplatin was associated with a 14% pathological complete response rate.[40]
- 2020 meta-analysis of 14 studies for NAC in UTUC found that the pooled pathologic complete response rate (≤ypT0N0M0) was 11% and pathologic partial response rate (≤ypT1N0M0) was 43%.[41]
- In the neoadjuvant setting, dosing regimens may be better tolerated, allowing more courses to be completed, and permitting patients to proceed to appropriate surgical intervention.
- A disadvantage of adjuvant chemotherapy is that many patients have baseline chronic kidney disease, which worsens after nephroureterectomy, rendering them ineligible to receive the full-dose cisplatinum-based chemotherapy
- Alternatives to cisplatin-based chemotherapy (i.e., immune checkpoint inhibitors, carboplatin, antibody drug conjugates, targeted FGFR therapies) are not recommended in the neoadjuvant setting (prior RNU or ureterectomy) outside of clinical trials
- Adjuvant
- Chemotherapy
- Platinum-based adjuvant chemotherapy should be offered to patients with advanced pathological stage (pT2–T4 pN0–N3 M0 or pTany N1–3 M0) UTUC after RNU or ureterectomy who have not received neoadjuvant platinum-based therapy[42]
- Adjuvant platinum-based chemotherapy for select patients with UTUC post-RNU is a standard based on results from the randomized phase III POUT trial.
- POUT
- Population: 260 patients with histologically confirmed pT2-T4, N0-3, M0 or pTany, N+, MO UTUC
- Pathological T stage: pT2 in 28%, pT3 in 66%, and pT4 in 6%
- Nodal stage: N0 in 91%, N1 in 6%, N2 in 3%, N3 in <1%
- Site of tumour: renal pelvis in 35%, ureter in 34%, both renal pelvis and ureter in 30%, and missing data in 1%
- GFR: 30–49 in 36%, ≥50 in 64%
- Randomized to 4 cycles of gemcitabine-cisplatin (gemcitabine-carboplatin if GFR 30-49ml/min) or surveillance with subsequent chemotherapy, if required
- Primary outcome: disease-free survival
- Secondary endpoints included metastasis-free survival, overall survival, toxicity & quality of life
- Results
- Trial closed early as data met early stopping rule for efficacy
- Median follow-up: 30 months
- Disease-free survival improved by 21% at 3 years (71% chemotherapy vs. 46% surveillance; HR 0.45)
- Significantly improved metastasis-free survival; OS data not mature
- Toxicity: neutropenia, thrombocytopenia, nausea, febrile neutropenia, vomiting; QOL worse initially with chemotherapy, similar by 6 monthsA subgroup analysis demonstrated that outcomes for patients with lymph node involvement and those treated with carboplatin chemotherapy were worse than those without positive nodes or treated with cisplatin chemotherapy
- Carboplatin remains a reasonable choice for HR cisplatin-ineligible patients post-RNU if NAC was not given
- Birtle, Alison, et al. "Adjuvant chemotherapy in upper tract urothelial carcinoma (the POUT trial): a phase 3, open-label, randomised controlled trial." The Lancet (2020).
- Population: 260 patients with histologically confirmed pT2-T4, N0-3, M0 or pTany, N+, MO UTUC
- POUT
- Adjuvant platinum-based chemotherapy for select patients with UTUC post-RNU is a standard based on results from the randomized phase III POUT trial.
- Immunotherapy
- Adjuvant nivolumab therapy may be offered to patients who received neoadjuvant platinum-based chemotherapy (ypT2–T4 or ypN+) or who are ineligible for or refuse perioperative cisplatin (pT3, pT4a, or pN+)[43]
- CheckMate 274 evaluated adjuvant nivolumab following surgery in patients with HR non-metastatic urothelial carcinoma
- Majority of patients underwent radical cystectomy for bladder primaries, 20% of patients underwent surgery for UTUC
- Inclusion criteria for both studies were patients with HR urothelial cancer defined as pT3, pT4a, or pN+ for patients who had not received neoadjuvant cisplatin-based chemotherapy and ypT2 to ypT4a or ypN+ for patients who had received neoadjuvant cisplatin
- Adjuvant nivolumab approved for UTUC and urothelial carcinoma of the bladder in patients with advanced disease identified from post-surgical pathology findings
- CheckMate 274 evaluated adjuvant nivolumab following surgery in patients with HR non-metastatic urothelial carcinoma
- Adjuvant platinum-chemotherapy over adjuvant nivolumab is recommended for eligible patients who did not receive NAC.
- Scenarios for use of adjuvant nivolumab include:[44]
- Patients with contraindications to platinum-based chemotherapy (e.g., poor renal function, performance status, sensorineural hearing loss, neuropathy or congestive heart failure, allergy)
- Patients with HR pathology after NAC
- Patients who refuse standard forms of adjuvant chemotherapy after appropriate counseling.
- Adjuvant nivolumab therapy may be offered to patients who received neoadjuvant platinum-based chemotherapy (ypT2–T4 or ypN+) or who are ineligible for or refuse perioperative cisplatin (pT3, pT4a, or pN+)[43]
- Radiation
- Radical nephroureterectomy alone provides a high rate of local control; adjuvant radiation without chemotherapy for high-stage disease does not protect against a high rate of distant failure
- Retrospective studies suggest that there may be a role for combined radiation-chemotherapy regimens in patients with advanced disease with adverse features
- Platinum-based adjuvant chemotherapy should be offered to patients with advanced pathological stage (pT2–T4 pN0–N3 M0 or pTany N1–3 M0) UTUC after RNU or ureterectomy who have not received neoadjuvant platinum-based therapy[42]
- Chemotherapy
Special scenarios[edit | edit source]
CIS of the Upper Urinary Tracts[edit | edit source]
- In most cases, the diagnosis is one of exclusion wherein there is a persistent positive selective cytology in the absence of any ureteroscopic or radiographic findings.
- The diagnosis of CIS of the upper urinary tracts difficult because of the inability to evaluate the urothelium of the upper tracts with adequate tissue samples
- Management
- Not well established
- Current approaches for presumed upper tract CIS include topical immunotherapy or chemotherapy
- Most experience is from use of BCG via a nephrostomy tube for primary treatment of CIS.
- Systematic review and meta-analysis evaluating intraluminal therapy for UTUC (2019)
- Inclusion criteria: studies evaluating patients with upper tract urothelial carcinoma receiving instillation treatment as adjuvant/curative therapy for pTa/pT1 and CIS, respectively.
- Studies with ≥10 participants included in quantitative analyses
- Results
- Included 226 patients from 15 studies of patients that underwent BCG instillation for CIS
- Recurrence-free survival: 84%
- Cancer-specific survival: 34%
- Overall survival: 16%
- No difference in survival based on approach (antegrade, retrograde, or combined) or drug (MMC vs. BCG)
- Foerster, Beat, et al. "Endocavitary treatment for upper tract urothelial carcinoma: a meta-analysis of the current literature." Urologic Oncology: Seminars and Original Investigations. Vol. 37. No. 7. Elsevier, 2019.
- Systematic review and meta-analysis evaluating intraluminal therapy for UTUC (2019)
- Historically, radical nephroureterectomy was performed for a unilateral cytologic abnormality of the upper tract to eliminate presumed CIS. This practice is not recommended in the absence of any histologic, radiographic, or endoscopic finding owing to the limitations of cytology alone with false-positive results and the high risk for bilateral disease in the future
- Observation is also not appropriate without further evaluation given the repeated abnormal cytologies.
- Most experience is from use of BCG via a nephrostomy tube for primary treatment of CIS.
- Management of CIS of ureteral margins during radical cystectomy is controversial
CIS limited to the region within the ureteral orifice[edit | edit source]
- Topical therapies such as BCG along with refluxing ureteral stenting that has been used for in cases of CIS near the ureterovesical junction or transurethral resection of the transmural portion of the ureter for very distal tumors, as an extension of bladder resection procedures, when tumor is limited to the region inside the ureteral orifice and not beyond the bladder wall, thus anatomically managed as bladder cancer
Watchful waiting or surveillance[edit | edit source]
- May be offered to select patients with UTUC with
- Significant comorbidities/competing risks of mortality
- Significant risk of End-Stage Renal Disease (ESRD) with any intervention resulting in dialysis.
- Discussion of treatment related risks including perioperative mortality may lead to a shared decision to proceed with active surveillance (whereby periodic assessments such as imaging or limited endoscopic assessment are performed) or watchful waiting/expectant management, where interventions are limited to palliation or awaiting symptomatic progression – especially in those with very limited life expectancy.
- In such cases, patients and family should be counseled and prepared for disease-related events such as bleeding, obstruction, infection, and pain with options for palliation that may be limited.
Advanced disease[edit | edit source]
Clinical, regional node-positive (N+)[edit | edit source]
- Should initially be treated with systemic therapy.
- Consolidative RNU or ureterectomy with lymph-node dissection may be performed in those with a partial or complete response.
- Pooled data from comparative outcomes utilizing NAC in patients with clinically node positive (cN+) disease supports this approach.
Distant metastatic disease (M+)[edit | edit source]
- Systemic therapy and alternative approaches (i.e., radiotherapy with or without chemotherapy in selected cases) should be favored for inoperable or symptomatic patients with M+ UTUC
- RNU or ureterectomy should not be offered as initial therapy
- Oncologic outcomes in the metastatic setting are strongly determined by response to systemic therapy, and surgical treatment has no demonstrable therapeutic efficacy for cytoreduction or as a single modality in this setting.
- Limited data on the efficacy of chemotherapy in metastatic UTUC
- Prospective randomized trials comparing chemotherapeutic regimens for UTUC are not feasible owing to the rarity of these patients.
- Regimen: MVAC (methotrexate, vinblastine, doxorubicin (Adriamycin), and cisplatin)
- Continues to have the highest response rate
- Carboplatin is frequently substituted instead of cisplatin because of either limitations of renal function or concerns over nephrotoxicity associated with cisplatin. Results with carboplatin are inferior than cisplatin.
- RNU or ureterectomy should not be offered as initial therapy
- Complete responses are rare in the metastatic setting, and the duration of response is limited, with overall survival of 12-24 months
Unresectable UTUC[edit | edit source]
- Localized disease may be deemed unresectable or ineligible for extirpative surgical management due to significant medical comorbidities or other factors including refusal to accept surgical treatment (e.g., solitary kidney).
- Should be offered a clinical trial or best supportive care including palliative management (radiation, systemic approach, endoscopic, or ablative) for refractory symptoms such as hematuria.
- Formulating alternative care options should be approached with multi-disciplinary input with a focus on realistic goals of care such as providing means of local control for functional preservation (e.g., renal function) and palliation (e.g., bleeding, infection)
- Multi-modal approaches include combination of endoscopic management to maintain upper and lower tract function (e.g., stents, nephrostomies, ablation for bleeding and local control) in addition to systemic treatment options if available. Rarely, radiation, angioembolization, or percutaneous ablation for palliation of bleeding can be offered
Prognosis[edit | edit source]
- 5-year overall survival rates:
- Grade
- 1-2: 40-87%
- 3-4: 0-33%
- Stage
- Ta, T1, CIS: 60-90%
- T2: 43-75%
- T3: 16-33%
- T4: 0-5%
- N+: 0-4%
- M+: 0%
- Grade
- Prognostic factors
- Tumour factors
- Stage
- Most important prognostic factor
- Non–organ confined disease (>pT2) is the most significant predictor of the development of metastases
- Most important prognostic factor
- Grade
- High-grade tumours are more likely to:
- Invade into the underlying connective tissue, muscle, and surrounding tissues
- Be associated with concomitant CIS
- While there is strong correlation between stage and grade, each independently predicts post-operative recurrence
- High-grade tumours are more likely to:
- Architecture
- ≈85% of renal pelvic tumors are papillary and the remainder sessile
- Papillary tumors seem to have better outcomes than sessile lesions
- Invasion of the lamina propria or muscle (stage T1 or T2) occurs in 50% of papillary and in >80% of sessile tumors
- CIS of the upper tract is associated with higher risk for disease progression (similar to bladder cancer) and a likelihood of future development of invasive urothelial cancers.
- Size
- Tumours > 3-4 cm may be associated with worse survival as well as a higher risk of bladder recurrence
- Location
- Renal pelvic tumours are usually more aggressive than ureteral tumours
- 50-60% of renal pelvic tumors are invasive into either the lamina propria or muscle, in contrast to most bladder tumors, which are usually non-invasive
- 55-75% of ureteral tumors are low grade and low stage, but invasion is still more common than bladder tumors
- The renal parenchyma may be a barrier, slowing distant spread of stage T3 renal pelvis tumors. In contrast, periureteral tumor extension carries a high risk of early tumor dissemination along the periureteral vascular and lymphatic supply. Improved survival of patients with stage T3 renal pelvis tumors versus ureteral tumors has been reported
- Conflicting results on whether the location of an upper tract tumor affects prognosis
- Renal pelvic tumours are usually more aggressive than ureteral tumours
- Multifocality
- Defined as presence of tumor in ≥2 sites within urothelium
- Independent predictor of poor clinical outcome
- Tumour necrosis
- Conflicting evidence on the influence of tumour necrosis on survival
- Lymph node involvement
- Although lymphadenectomy is seldom performed for clinically node-negative disease, pathologic lymph node status is a strong predictor of post-nephroureterectomy recurrence
- LVI
- Associated with worse survival in patients without positive nodes; no association in N+ disease
- Hydronephrosis
- Independently associated with advanced disease stage and poor survival
- Positive surgical margins
- Previous or concomitant bladder tumours
- Stage
- Patient factors
- Age
- Increasing age associated with worse survival
- Race
- Black non-Hispanic race is associated with increased mortality
- Age
- Surgical factors
- Lack of post-operative mitomycin C instillation
- Tumour factors
- 3 particular forms of UTUC, 2 associated with environmental exposure (aristolochic acid nephropathy, which includes Balkan and Chinese herbal nephropathy, as well as those seen in arsenic-endemic regions), analgesic abuse, and those associated with Lynch syndrome, have an even higher tendency have multiple and bilateral recurrences than do sporadic tumors
Surveillance and Survivorship
Oncologic Surveillance[edit | edit source]
- The primary aims of postoperative surveillance for UTUC are to identify
- Urothelial recurrences
- De novo tumours of the urinary tract
- Regional/distant metastases at early stages when they may be amenable to treatment
- Recurrence after
- Nephron-sparing approaches
- Most patients following nephron-sparing procedures will develop ipsilateral upper tract recurrences.
- Ipsilateral upper tract tumor usually occurs in a proximal-to-distal direction; recurrence proximal to the original lesion is rare.
- This high rate of ipsilateral recurrence results in part from a multifocal field change, which is even more pronounced than in bladder cancer
- Most patients following nephron-sparing procedures will develop ipsilateral upper tract recurrences.
- Nephroureterectomy
- Intravesical recurrence
- ≈30% patients with UTUC will subsequently develop bladder cancer after nephroureterectomy or nephron-sparing procedures
- Most recurrences occur within the first 2 years
- Median time to bladder recurrence 6-12 months
- Unclear how long bladder surveillance should continue for after 2 years
- Given the high incidence of metachronous bladder involvement, routine bladder surveillance should be performed in patients with a history of UTUC
- Potential explanations on why bladder cancers following UTUC are more common than UTUC following bladder cancer include:
- Downstream seeding
- Longer exposure time to carcinogens in the bladder
- Greater number of urothelial cells in the bladder that are subject to random carcinogenic events
- Most recurrences occur within the first 2 years
- Risk factors for intravesical recurrence:
- Male sex
- Previous bladder cancer
- Preoperative CKD
- Positive preoperative urinary cytology
- Ureteral tumor size
- Multifocality
- Invasive pathologic T-stage
- Presence of necrosis
- Laparoscopic approach
- Extravesical bladder cuff removal
- Positive surgical margins
- Prior ureteroscopic biopsy
- Given the substantial risk of local (bladder) recurrences within the first years following nephroureterectomy, risk adapted surveillance with cystoscopy and urine cytology at routine intervals is indicated to facilitate prompt detection of bladder recurrences.
- ≈30% patients with UTUC will subsequently develop bladder cancer after nephroureterectomy or nephron-sparing procedures
- Contralateral recurrence
- Risk of recurrence to the contralateral upper tract: ≈2%
- Locoregional, retroperitoneal, and distant metastases
- Risk factors
- Multifocality
- Stage T3-4
- Grade G3
- Presence of lymph node metastasis
- Intrabdominal recurrences
- Very low rates in low-risk patients
- Retroperitoneum or pelvis occurred in ≈5%
- In patients with HG disease, LVI, or tumor multifocality, periodic imaging of the abdomen and pelvis is warranted, particularly for the first 2 years
- Very low rates in low-risk patients
- Port-site occur very infrequently, usually associated with inadvertent entry into the collecting system.
- Distant metastases
- Occurred following nephroureterectomy in 16% of patients.
- Median time to metastases was 13-16 months.
- Location of metastases
- Lung metastasis (5%)
- Low risk in patients with <pT2 N0/M0
- Can occur in patients with high-grade disease, so periodic chest imaging is warranted
- Chest imaging can be done via chest x-ray or CT
- Chest x-ray is likely sufficient, less costly, and associated with less radiation exposure
- Chest imaging can be done via chest x-ray or CT
- Bone (4%)
- Liver (4%)
- Brain
- Rare following nephroureterectomy
- Patients undergoing follow-up for HR UTUC following nephroureterectomy with acute neurological signs or symptoms should undergo prompt neurologic evaluation with cross-sectional imaging of the brain and/or spine by CT or MRI
- Adrenal gland
- Non-regional lymph nodes
- Lung metastasis (5%)
- Risk factors
- Intravesical recurrence
- Nephron-sparing approaches
- Post-operative evaluation must routinely include evaluation of the:
- Bladder, through
- Cystoscopy
- Ipsilateral (if organ-sparing therapy was chosen) and contralateral urinary tracts, through
- Upper tract endoscopy
- Upper tract imaging
- Preferred modality: CT urogram
- If patient unable to receive iodinated contrast, use MR urography or retrograde pyelography combined with non-contrast axial imaging
- Preferred modality: CT urogram
- Urine cytology
- Extra-urinary sites for local and metastatic spread, through
- CXR or CT chest
- Bladder, through
Schedule[edit | edit source]
AUA[edit | edit source]
- See Table from Original Guidelines
Surveillance after kidney sparing[edit | edit source]
- Low-risk patients managed with kidney sparing treatment
- Cystoscopy and upper tract endoscopy within 1-3 months of treatment to confirm successful treatment.
- If successful treatment confirmed (no evidence of disease), perform
- Cystoscopy of the bladder once again within the first year after treatment, then at least every 6-9 months for the first 2 years and then at least annually thereafter.
- Upper tract endoscopy at 6 months and 1 year [after treatment].
- Can be subsequently performed for any symptoms or significant findings on upper tract imaging.
- Upper tract imaging should be performed at least every 6-9 months for first 2 years, then annually up to 5 years.
- Surveillance after 5 years in the absence of recurrence should be based on shared decision-making.
- Upper tract endoscopy at 6 months and 1 year [after treatment].
- Cystoscopy of the bladder once again within the first year after treatment, then at least every 6-9 months for the first 2 years and then at least annually thereafter.
- No distant metastatic evaluation since risk is low with low-risk disease
- High-risk patients managed with kidney sparing treatment
- Cystoscopy, upper tract endoscopy, and upper tract urine cytology within 1-3 months of treatment to confirm successful treatment.
- If successful treatment confirmed (no evidence of disease), perform
- Cystoscopy of the bladder and cytology at least every 3-6 months for the first 3 years and then every 6-12 months up to 5 years.
- Upper tract endoscopy should be performed at least at 6 months and 1 year [after treatment]
- Upper tract imaging and BMP should be performed every 3-6 months for 3 years, then every 6-12 months for 2 years, and then annually thereafter.
- Distant metastatic evaluation: Chest imaging (chest X-ray or CT) is recommended every 6-12 months to evaluate for intrathoracic metastasis up to 5 years following last diagnosis/treatment
- Surveillance after 5 years in the absence of recurrence should be based on shared decision-making.
- If patient develops urothelial recurrence in the bladder or urethra or positive cytology following kidney sparing treatment for UTUC, evaluate for possible ipsilateral recurrence or development of new contralateral upper tract disease.
Surveillance after radical nephroureterectomy[edit | edit source]
- <pT2 N0/M0 managed with NU
- Cystoscopy and urine cytology within 3 months after surgery, then repeated based on pathologic grade.
- For LG this should repeated at least every 5-9 months for the first 2 years and then at least annually thereafter.
- For HG, this should be repeated at least every 3-6 months for the first 3 years and then at least annually thereafter.
- Cross-sectional imaging of the abdomen and pelvis should be done within 6 months after surgery and then at least annually for a minimum of 5 years***Due to the metastasis risk and estimated 5% probability for contralateral disease
- Follow up after nephroureterectomy for patients with non-muscle invasive, node-negative UTUC should be largely focused on the risk of intravesical recurrence
- Surveillance after five years in the absence of recurrence should be encouraged and based on shared decision-making between the patient and clinician
- Cystoscopy and urine cytology within 3 months after surgery, then repeated based on pathologic grade.
- T2+ managed with NU
- Cystoscopy with cytology at 3 months after surgery, then every 3-6 months for 3 years, and then annually thereafter.
- Cross-sectional imaging of the abdomen and pelvis with multiphasic contrast-enhanced CT urography should be performed every 3-6 months for years 1 and 2, every 6 months at year 3, and annually thereafter to year 5.
- Chest imaging, preferably with chest CT, every 6-12 months for the first 5 years.
- Beyond five years after surgery in patients without recurrence, ongoing surveillance with cystoscopy and upper tract imaging may be continued on an annual basis according to principles of shared/informed decision-making
- Sequelae of nephroureterectomy
- Repeat assessment of blood pressure, eGFR, and proteinuria should be performed soon after nephroureterectomy then again in 3-6 months to assess for development or progression of CKD.
- With significant nephron mass loss, hyperfiltration can occur resulting in glomerular damage, exacerbation of proteinuria and progressive sclerosis with further decline in GFR.
- The long-term impact of renal dysfunction increases risks of osteoporosis, anemia, metabolic and cardiovascular disease, hospitalization and death.
- Effective treatment strategies are available to slow the progression of CKD and reduce cardiovascular risks, and therefore timely identification of progressive renal dysfunction and/or proteinuria can provide opportunity for medical intervention when indicated.
- Careful management of DM and HTN and avoidance of substantial weight gain may slow or prevent CKD progression and should be prioritized on a long-term basis
- Identifying modifiable risk factors including diabetes mellitus (DM), hypertension (HTN) and smoking is essential. Optimizing glycemic and blood pressure control, smoking cessation and minimizing risk of acute kidney injury (with avoidance of hypotension and nephrotoxic agents such as intravenous contrast or non-steroidal anti-inflammatory drugs) should reduce the degree of renal dysfunction in the perioperative period.
- In patients who develop progressive renal insufficiency or proteinuria should be referred to nephrology.
- Other laboratory evaluations (e.g., CBC, LDH, liver function tests, and alkaline phosphatase) may be obtained at the discretion of the clinician or if advanced disease is suspected.
- Repeat assessment of blood pressure, eGFR, and proteinuria should be performed soon after nephroureterectomy then again in 3-6 months to assess for development or progression of CKD.
CUA[edit | edit source]
- See Table from 2018 CUA Surveillance guidelines based on recurrence patterns for upper tract urothelial carcinoma
- Bladder
- Should be assessed with cytology and cystoscopy in all patients at months 3, 6, 12, 18, 24 and annually thereafter for up to 10 years of recurrence-free survival
- Ipsilateral upper tract
- Should be assessed by URS and selective cytology or biopsy in all patients following nephron-sparing procedures at months 3, 6, 12, 18, 24 and annually thereafter up to 10 years of recurrence-free survival
- Computed tomography urography (CTU) and retrograde pyelography lacks sensitivity
- Should be assessed by URS and selective cytology or biopsy in all patients following nephron-sparing procedures at months 3, 6, 12, 18, 24 and annually thereafter up to 10 years of recurrence-free survival
- Extra-urinary sites
- Routine blood work should include:
- Renal function tests
- Metabolic panel, including liver function tests, calcium and alkaline phosphatase
- To assess for local, contralateral and distant metastases in patients after nephroureterectomy or nephron-sparing procedures, imaging of the abdomen and pelvis with CTU is recommended
- MRI or US may be substituted for CTU in patients with contraindications to CTU
- CXR is recommended to assess for lung metastases
- Bone scan is indicated in the presence of bone pain, elevated calcium or elevated alkaline phosphatase to assess for bone metastases
- Routine blood work should include:
- Lack of evidence for an optimal duration of surveillance; recommended approach:
- High-grade, pT≥2 or pN+: lifelong annual surveillance with history, physical examination, blood work, urine cytology and abdominal/chest imaging
- Low-grade, pT<2 pN0/x: annual cystoscopy and ipsilateral ureteroscopy (following nephron-sparing procedures) may be omitted after 10 years of recurrence-free survival; after 10 years of recurrence-free survival, patients with may be discharged from annual surveillance
Survivorship[edit | edit source]
- Discuss disease-related stresses and risk factors and encourage patients with urothelial cancer to adopt healthy lifestyle habits, including smoking cessation, exercise, and a healthy diet, to promote long-term health benefits and quality of life.
- UTUC is associated with metabolic syndrome and obesity, with obesity adversely impacting disease-specific outcomes among patients undergoing RNU.
- Clinicians should work with patients and their primary care providers to ensure that comorbidities are optimally managed throughout the course of care for UTUC and during surveillance to maximize quality of life during survivorship.
Questions
- What are the risk factors for upper tract urothelial carcinoma (UTUC)?
- Which other malignancies are associated with Lynch syndrome?
- In patients with bladder cancer, what is the risk of subsequent UTUC? In patients with UTUC, what is the risk of subsequent bladder cancer?
- in patients that have undergone cystectomy for bladder cancer, which of the following is not a risk factor for subsequent UTUC?
- What is the most important predictor of developing metastasis?
- What is the differential diagnosis of a filling defect in the collecting system?
- What is the most important prognostic factor for survival in UTUC?
- What are the indications for nephroureterectomy? Segmental ureterectomy?
Answers
- What are the risk factors for upper tract urothelial carcinoma (UTUC)?
- Smoking
- Occupational exposure
- Chronic inflammation
- Cyclophosphamide exposure
- Analgesic abuse
- Lynch syndrome
- Exposure to aristolocholic acid (Balkan nephropathy)
- Exposure to arsenic
- Which other malignancies are associated with Lynch syndrome?
- Colonic (most common), endometrial (second most common), prostate, urothelial, adrenal, gastric, pancreatic, uterine, ovarian, and sebaceous carcinomas
- In patients with bladder cancer, what is the risk of subsequent UTUC? In patients with UTUC, what is the risk of subsequent bladder cancer?
- 2-4% patients with bladder cancer will subsequently develop UTUC,
- ≈30% patients with UTUC will subsequently develop bladder cancer after nephroureterectomy or nephron-sparing procedures
- In patients that have undergone cystectomy for bladder cancer, which of the following is not a risk factor for subsequent UTUC?
- Presence of CIS
- N0 status
- High-grade tumours
- Involvement of male prostatic urethra or female urethra
- What is the most important predictor of developing metastasis?
- T stage > 2
- What is the differential diagnosis of a filling defect in the collecting system?
- Tumour
- Blood clot
- Stone
- Sloughed papilla
- Fungus ball
- Overlying bowel gas
- External compression
- What is the most important prognostic factor for survival in UTUC?
- Stage; recall in bladder grade has stronger association with progression of NMIBC than stage
- What are the indications for nephroureterectomy? Segmental ureterectomy?
- Nephroureterectomy: high-grade or pT2
- Segmental ureterectomy:
- Low-grade, low-stage tumors that are not able to be removed endoscopically because of tumor size or multiplicity
- High-grade or invasive tumors when preservation of renal unit is necessary
References
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, vol 1, chap 58
- Coleman, Jonathan A., et al. "Diagnosis and Management of Non-Metastatic Upper Tract Urothelial Carcinoma: AUA/SUO Guideline." The Journal of Urology 209.6 (2023): 1071-1081.