Abdominal Wall: Difference between revisions
Jump to navigation
Jump to search
Urology4all (talk | contribs) |
Urology4all (talk | contribs) |
||
| (5 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
=== Layers === | === Layers === | ||
* | * <span style="color:#ff0000">'''vFrom superficial to deep'''</span> | ||
** | ** <span style="color:#ff0000">'''Skin'''</span> | ||
*** | *** <span style="color:#ff0000">'''Camper fascia'''</span> | ||
*** | *** <span style="color:#ff0000">'''Scarpa fascia'''</span> | ||
** | ** <span style="color:#ff0000">'''Abdominal musculature'''</span> | ||
*** | *** <span style="color:#ff0000">'''External oblique'''</span> | ||
*** | *** <span style="color:#ff0000">'''Internal oblique'''</span> | ||
*** | *** <span style="color:#ff0000">'''Transversus abdominis'''</span> | ||
** | ** <span style="color:#ff0000">'''Transversalis fascia'''</span> | ||
** | **<span style="color:#ff0000">'''Peritoneum'''</span> | ||
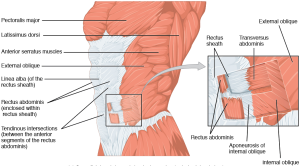
[[File:1112 Muscles of the Abdomen Anterolateral.png|thumb|[[commons:File:1112_Muscles_of_the_Abdomen_Anterolateral.png|Source]]]] | |||
=== Skin and subcutaneous fasciae === | === Skin and subcutaneous fasciae === | ||
==== Camper fascia ==== | |||
* '''A loose layer of fatty tissue deep to the skin''' | |||
* Varies in thickness with the nutritional status of the patient | |||
* <span style="color:#ff0000">'''Some branches from the femoral vessels'''</span> (superficial circumflex iliac, external pudendal, and superficial inferior epigastric vessels)<span style="color:#ff0000"> '''run in this layer'''</span> | |||
* ''' | ** '''<span style="color:#ff0000">Clinical implication: The superficial inferior epigastric vessels are encountered during inguinal incisions and can cause troublesome bleeding during placement of pelvic laparoscopic ports</span>''' | ||
==== Scarpa fascia ==== | |||
* '''Dense collagenous connective tissue layer[https://www.ncbi.nlm.nih.gov/books/NBK553137/]''' | |||
*'''Deep to Camper fascia''' | |||
*'''Considerably thinner than Camper's fascia[https://www.ncbi.nlm.nih.gov/books/NBK553137/]''' | |||
**although it may be difficult to discern in older patients | |||
* '''<span style="color:#ff0000">Continuous with (5):</span>''' | |||
*# '''Camper fascia superiorly and laterally''' | |||
*# '''Deep fascia of the thigh (fascia lata) laterally''', 1 cm below the inguinal ligament along a line from the anterior superior iliac spine to the pubic tubercle | |||
*# '''<span style="color:#ff0000">Colles fascia of the perineum medially</span>''' | |||
*# '''<span style="color:#ff0000">Dartos fascia of the penis</span>''' | |||
*# '''<span style="color:#ff0000">Dartos smooth muscle of the scrotum</span>'''. | |||
** '''<span style="color:#ff0000">Clinical implication: the continuity of these fasciae can limit both the spread of infection in necrotizing fasciitis of the scrotum (Fournier gangrene), hematoma from injury, and the extent of urinary extravasation in an anterior urethral injury.</span>''' | |||
*** '''<span style="color:#ff0000">Because of these fasciae, bleeding, infection, or urinary extravasation will not extend down the leg or into the buttock but can freely travel up the anterior abdominal wall deep to Scarpa fascia to the clavicles</span>'''§ '''and around the flank to the back. In the perineum, their spread is limited by the fusions of Colles fascia''' to the ischiopubic rami laterally and to the posterior edge of the perineal membrane; '''the resulting hematoma is therefore butterfly shaped.''' | |||
*** '''The external, cremasteric, and internal spermatic fasciae are embryologically distinct from the scrotal and dartos layers and have their own blood and nerve supplies. It is uncommon for them to be involved in the necrotic process in Fournier gangrene; therefore they can be spared. (In practice, all scrotal tissue is debrided to the tunica vaginalisin patients with Fournier gangrene)'''. | |||
=== Abdominal musculature === | === Abdominal musculature === | ||
| Line 67: | Line 73: | ||
== Inguinal canal == | == Inguinal canal == | ||
* '''Transmits (2):''' | * '''<span style="color:#ff0000">Transmits (2):</span>''' | ||
** '''Ilioinguinal nerve (L1)''' | ** '''<span style="color:#ff0000">Ilioinguinal nerve (L1)</span>''' | ||
** '''Spermatic cord/round ligament''' | ** '''<span style="color:#ff0000">Spermatic cord/round ligament</span>''' | ||
* '''Anterior wall and floor (inferior wall): external oblique, which folds over at its inferior edge as the inguinal ligament''' | * '''<span style="color:#ff0000">Anterior wall and floor (inferior wall): external oblique, which folds over at its inferior edge as the inguinal ligament</span>''' | ||
* '''Posterior wall: transversalis fascia''' | * '''<span style="color:#ff0000">Posterior wall: transversalis fascia</span>''' | ||
* '''Roof (superior wall): fibers of the internal oblique and transversus abdominis''' | * '''<span style="color:#ff0000">Roof (superior wall): fibers of the internal oblique and transversus abdominis</span>''' | ||
* External inguinal ring | * External inguinal ring | ||
** Invaginate the scrotum with a finger to identify approximate location | ** Invaginate the scrotum with a finger to identify approximate location | ||
| Line 83: | Line 89: | ||
*** '''Above the inguinal ligament''' | *** '''Above the inguinal ligament''' | ||
*** '''Lateral to inferior epigastric vessels''' | *** '''Lateral to inferior epigastric vessels''' | ||
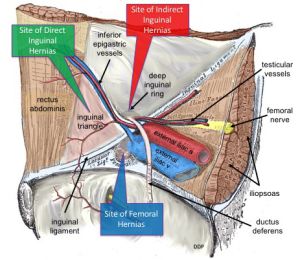
**** Cord structures pierce the fascia lateral to the inferior epigastric vessels at the internal inguinal ring. | **** Cord structures pierce the fascia lateral to the inferior epigastric vessels at the internal inguinal ring.[[File:Common Sites of Lower Abdominal Hernias.jpg|thumb|[[commons:File:Common_Sites_of_Lower_Abdominal_Hernias.jpg|Source]]]] | ||
* Conjoint tendon | *Conjoint tendon | ||
** Formed by the fusion of the internal oblique and the transversalis fascia | ** Formed by the fusion of the internal oblique and the transversalis fascia | ||
** Reinforces the posterior wall of the inguinal canal. | ** Reinforces the posterior wall of the inguinal canal. | ||
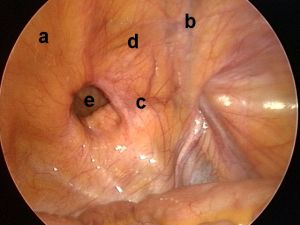
* '''Hernias into the canal may occur medial (direct) or lateral (indirect) to the inferior epigastric vessels''' | * '''Hernias into the canal may occur medial (direct) or lateral (indirect) to the inferior epigastric vessels''' | ||
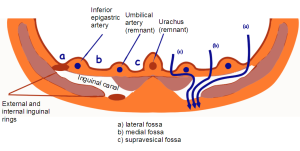
* '''Internal surface of the anterior abdominal wall''' | * '''Internal surface of the anterior abdominal wall''' | ||
** '''Approached laparoscopically, 3 elevations of the peritoneum, referred to as the median, medial, and lateral umbilical folds, are visible on the anterior abdominal wall below the umbilicus:''' | ** '''Approached laparoscopically, 3 elevations of the peritoneum, referred to as the median, medial, and lateral umbilical folds, are visible on the anterior abdominal wall below the umbilicus:''' | ||
| Line 95: | Line 100: | ||
*** '''The medial umbilical fold contains the obliterated umbilical artery''' and serves as an important landmark for the surgeon as it may be traced to its origin from the internal iliac artery to locate the ureter, which lies on its medial side. During the performance of transperitoneal laparoscopic or robotic radical prostatectomy, the medial umbilical folds are used as landmarks to guide the dissection of the bladder to expose the space of Retzius. | *** '''The medial umbilical fold contains the obliterated umbilical artery''' and serves as an important landmark for the surgeon as it may be traced to its origin from the internal iliac artery to locate the ureter, which lies on its medial side. During the performance of transperitoneal laparoscopic or robotic radical prostatectomy, the medial umbilical folds are used as landmarks to guide the dissection of the bladder to expose the space of Retzius. | ||
*** '''The lateral umbilical fold contains the inferior epigastric vessels''' as they ascend to supply the rectus abdominis. | *** '''The lateral umbilical fold contains the inferior epigastric vessels''' as they ascend to supply the rectus abdominis. | ||
[[File:Inguinal fossae.png|thumb|[[commons:File:Inguinal_fossae.PNG|Source]]]] | [[File:Inguinal fossae.png|thumb|[[commons:File:Inguinal_fossae.PNG|Source]]]][[File:Laparoscopic view of inguinal region.jpg|thumb|Laparoscopic view of anterior abdominal wall and pelvis, demonstrating a direct inguinal hernia. a: rectus abdominis; b: inferior epigastric artery; c: inguinal ligament; d: Hesselbach's triangle; e: inguinal hernia. [[commons:File:Laparoscopic_view_of_inguinal_region.jpg|Source]]]] | ||
== Questions == | == Questions == | ||
Latest revision as of 18:04, 18 July 2024
Anterior abdominal wall[edit | edit source]
Layers[edit | edit source]
- vFrom superficial to deep
- Skin
- Camper fascia
- Scarpa fascia
- Abdominal musculature
- External oblique
- Internal oblique
- Transversus abdominis
- Transversalis fascia
- Peritoneum
- Skin
Skin and subcutaneous fasciae[edit | edit source]
Camper fascia[edit | edit source]
- A loose layer of fatty tissue deep to the skin
- Varies in thickness with the nutritional status of the patient
- Some branches from the femoral vessels (superficial circumflex iliac, external pudendal, and superficial inferior epigastric vessels) run in this layer
- Clinical implication: The superficial inferior epigastric vessels are encountered during inguinal incisions and can cause troublesome bleeding during placement of pelvic laparoscopic ports
Scarpa fascia[edit | edit source]
- Dense collagenous connective tissue layer[1]
- Deep to Camper fascia
- Considerably thinner than Camper's fascia[2]
- although it may be difficult to discern in older patients
- Continuous with (5):
- Camper fascia superiorly and laterally
- Deep fascia of the thigh (fascia lata) laterally, 1 cm below the inguinal ligament along a line from the anterior superior iliac spine to the pubic tubercle
- Colles fascia of the perineum medially
- Dartos fascia of the penis
- Dartos smooth muscle of the scrotum.
- Clinical implication: the continuity of these fasciae can limit both the spread of infection in necrotizing fasciitis of the scrotum (Fournier gangrene), hematoma from injury, and the extent of urinary extravasation in an anterior urethral injury.
- Because of these fasciae, bleeding, infection, or urinary extravasation will not extend down the leg or into the buttock but can freely travel up the anterior abdominal wall deep to Scarpa fascia to the clavicles§ and around the flank to the back. In the perineum, their spread is limited by the fusions of Colles fascia to the ischiopubic rami laterally and to the posterior edge of the perineal membrane; the resulting hematoma is therefore butterfly shaped.
- The external, cremasteric, and internal spermatic fasciae are embryologically distinct from the scrotal and dartos layers and have their own blood and nerve supplies. It is uncommon for them to be involved in the necrotic process in Fournier gangrene; therefore they can be spared. (In practice, all scrotal tissue is debrided to the tunica vaginalisin patients with Fournier gangrene).
Abdominal musculature[edit | edit source]
- Deep to Scarpa fascia
- Laterally, there are the external oblique, internal oblique, and transversus abdominis muscles; medially, there are the rectus abdominis and pyramidalis muscles.
- Laterally
- Superficial to deep:
- External oblique
- Internal oblique
- Transversus abdominis
- The external oblique, internal oblique, and transversus abdominis muscles terminate on the anterior abdominal wall as broad, tough aponeurotic sheets that fuse in the midline (linea alba) and form the anterior and posterior rectus sheaths
- The arcuate line/linea semicircularisis 2/3 of the distance between the pubis and the umbilicus
- Above the arcuate line:
- The anterior rectus sheath is formed by the aponeurosis of the external oblique muscle and a portion of the internal oblique muscle
- The posterior sheath is derived from the remaining internal oblique aponeurosis and the transversus abdominis aponeurosis
- Below the arcuate line:
- The anterior rectus sheath is formed by the aponeurosis of all the muscle layers
- The posterior sheath is absent; directly posterior to the rectus abdominus is transversalis fascia then peritoneum.
- Above the arcuate line:
- Superficial to deep:
- Medially
- The linea alba is avascular and is a convenient point of access to the peritoneal and extra-peritoneal pelvic cavities.
- Rectus abdominis
- Arises from the pubis medial to the pubic tubercle and inserts on the xiphoid process and adjacent costal cartilages
- Tendinous intersections connect it to anterior rectus sheath so rectus can be divided transversely without retracting
- Innervated by T6-12
- Pyramidalis
- Arises from the pubic crest and inserts into the linea alba
- Anterior to the rectus and within its sheath
- Triangle-shaped muscle
- Innervated by T12
Transversalis fascia[edit | edit source]
- Thin aponeurotic membrane between abdominal musculature and perietal peritoneum
Peritoneum[edit | edit source]
Inguinal canal[edit | edit source]
- Transmits (2):
- Ilioinguinal nerve (L1)
- Spermatic cord/round ligament
- Anterior wall and floor (inferior wall): external oblique, which folds over at its inferior edge as the inguinal ligament
- Posterior wall: transversalis fascia
- Roof (superior wall): fibers of the internal oblique and transversus abdominis
- External inguinal ring
- Invaginate the scrotum with a finger to identify approximate location
- Lateral edges (crura): fibers of the external oblique aponeurosis split above the pubic tubercle
- Superior edge: transverse (intercrural) fibers bridge the crura; by dividing the intracrural fibers, the external oblique can be separated along its fibers to gain access to the cord.
- Internal inguinal ring
- Location
- Midway between the anterior superior iliac spine and the pubic tubercle
- 4 cm lateral to the external ring
- Above the inguinal ligament
- Lateral to inferior epigastric vessels
- Cord structures pierce the fascia lateral to the inferior epigastric vessels at the internal inguinal ring.
Source
- Cord structures pierce the fascia lateral to the inferior epigastric vessels at the internal inguinal ring.
- Location
- Conjoint tendon
- Formed by the fusion of the internal oblique and the transversalis fascia
- Reinforces the posterior wall of the inguinal canal.
- Hernias into the canal may occur medial (direct) or lateral (indirect) to the inferior epigastric vessels
- Internal surface of the anterior abdominal wall
- Approached laparoscopically, 3 elevations of the peritoneum, referred to as the median, medial, and lateral umbilical folds, are visible on the anterior abdominal wall below the umbilicus:
- The median fold contains the median umbilical ligament (urachus), a fibrous remnant of the cloaca that attaches the bladder to the anterior abdominal wall.
- The medial umbilical fold contains the obliterated umbilical artery and serves as an important landmark for the surgeon as it may be traced to its origin from the internal iliac artery to locate the ureter, which lies on its medial side. During the performance of transperitoneal laparoscopic or robotic radical prostatectomy, the medial umbilical folds are used as landmarks to guide the dissection of the bladder to expose the space of Retzius.
- The lateral umbilical fold contains the inferior epigastric vessels as they ascend to supply the rectus abdominis.
- Approached laparoscopically, 3 elevations of the peritoneum, referred to as the median, medial, and lateral umbilical folds, are visible on the anterior abdominal wall below the umbilicus:
Questions[edit | edit source]
Answers[edit | edit source]
References[edit | edit source]
- Flynn, William, and Paula Vickerton."Anatomy, Abdomen and Pelvis, Abdominal Wall." (2019).
- Mahadevan, Vishy."Anatomy of the anterior abdominal wall and groin." Surgery-Oxford International Edition 24.7 (2006): 221-223.
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 68