Male Reproductive Physiology: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
****# Pulsatile, peaks every 90-120 minutes | ****# Pulsatile, peaks every 90-120 minutes | ||
****## Pulsatility arises at puberty, around age 12 | ****## Pulsatility arises at puberty, around age 12 | ||
[[File:Hypothalamic hormones.png|thumb|389x389px|Hormones produced by the hypothalamus and pituitary gland|center]] | [[File:Hypothalamic hormones.png|thumb|389x389px|Hormones produced by the hypothalamus and pituitary gland|center]]'''Anterior pituitary''' | ||
*'''Produces (6):''' | |||
*#'''Luteinizing hormone''' | |||
*#'''Follicle-stimulating hormone''' | |||
*#Growth hormone | |||
*#Thyroid-stimulating hormone | |||
*#Adrenocorticotropic hormone | |||
*#Prolactin | |||
*'''LH and FSH act only on gonads''' | |||
*'''Luteinizing hormone (LH)''' | |||
**'''Function:''' | |||
***'''Stimulates steroidogenesis within Leydig cells''' | |||
****'''Most important regulator of testosterone production''' | |||
*****'''Clinical implication: infertilty secondary to reduced LH can be treated with hCG hormonal therapy, which is an analogue of LH''' | |||
**'''Secretion''' | |||
***'''Regulated by negative feedback from estrogens (primary mechanism) and androgens''' | |||
****'''Estradiol feedback occurs mainly at pituitary''' but also negative-feedback on hypothalamus | |||
****'''Testosterone feedback occurs mainly at hypothalamus''' | |||
*****'''Clinical implication: exogenous testosterone inhibits production of FSH and LH and is associated with decreased serum FSH and LH''' | |||
*'''Follicle-stimulating hormone (FSH)''' | |||
**'''Function:''' | |||
***'''Stimulates Sertoli cells''' | |||
****'''Major stimulator of seminiferous tubule growth''' | |||
****'''Essential for initiation of spermatogensis at puberty''' '''but not essential for spermatogenesis in acquired infertility (i.e. after puberty)''' | |||
*****'''Clinical implication: infertilty can be treated with hCG hormonal therapy monotherapy without concomitant recombinant FSH''' | |||
**'''Secretion''' | |||
***'''Stimulated by (2):''' | |||
***#'''Estrogen''' | |||
***#'''Activin''' | |||
***'''Inhibited by (1):''' | |||
***#'''Inhibin''' | |||
***Thought to account for the '''relative secretory independence of FSH from GnRH secretion''' | |||
*'''Activin''' | |||
**'''Secreted by Leydig cells''' | |||
*'''Inhibin-B''' | |||
**'''Secreted by Sertoli cells''' | |||
**'''Production is stimulated by FSH''' | |||
**'''Acts by negative feedback at the pituitary''' [Campbell’s 12th edition, page 1319 says both “hypothalamus or pituitary”, [[wikipedia:Activin_and_inhibin#Inhibin|Wikipedia]] says “Inhibin does not inhibit the secretion of GnRH from the hypothalamus", 2019 AUA Update on Exogenous Testosterone and Male Reproduction agrees with Wikipedia] '''to inhibit FSH production''' | |||
*'''[https://pubmed.ncbi.nlm.nih.gov/2672952/ Inhibin and activin can influence steroid production by Leydig cells]'''<br /> | |||
*'''Prolactin''' | |||
**'''Normal levels may increase concentration of LH receptors on Leydig cells and sustain normal, high intratesticular testosterone levels''' | |||
**May also potentiate the effects of androgens on growth and secretions of male accessory sex glands | |||
**'''Hyperprolactinemia abolishes GnRH pulsatility and is a cause of infertility''' | |||
***'''See [[Testosterone Deficiency (2018)|2018 AUA T Deficiency Guideline Notes]]''' | |||
===== '''Testis''' ===== | |||
* '''See [[Testicle|Testis Anatomy]]''' '''Notes''' | |||
* After binding LH, Leydig cells transport cholesterol into mitochondria and produce testosterone. | |||
Revision as of 09:40, 27 August 2022
Components of the Reproductive (Hypothalamus, Pituitary, Testis) Axis
- Hypothalamus
- Produces GnRH
- GnRH
- Simulates production and release of LH and FSH from anterior pituitary
- Patterns of secretion (3):
- Seasonal (peaking in spring)
- Circadian (highest testosterone in morning)
- Pulsatile, peaks every 90-120 minutes
- Pulsatility arises at puberty, around age 12
- GnRH
- Produces GnRH
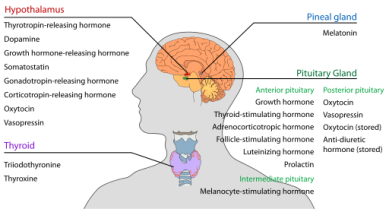
Anterior pituitary
- Produces (6):
- Luteinizing hormone
- Follicle-stimulating hormone
- Growth hormone
- Thyroid-stimulating hormone
- Adrenocorticotropic hormone
- Prolactin
- LH and FSH act only on gonads
- Luteinizing hormone (LH)
- Function:
- Stimulates steroidogenesis within Leydig cells
- Most important regulator of testosterone production
- Clinical implication: infertilty secondary to reduced LH can be treated with hCG hormonal therapy, which is an analogue of LH
- Most important regulator of testosterone production
- Stimulates steroidogenesis within Leydig cells
- Secretion
- Regulated by negative feedback from estrogens (primary mechanism) and androgens
- Estradiol feedback occurs mainly at pituitary but also negative-feedback on hypothalamus
- Testosterone feedback occurs mainly at hypothalamus
- Clinical implication: exogenous testosterone inhibits production of FSH and LH and is associated with decreased serum FSH and LH
- Regulated by negative feedback from estrogens (primary mechanism) and androgens
- Function:
- Follicle-stimulating hormone (FSH)
- Function:
- Stimulates Sertoli cells
- Major stimulator of seminiferous tubule growth
- Essential for initiation of spermatogensis at puberty but not essential for spermatogenesis in acquired infertility (i.e. after puberty)
- Clinical implication: infertilty can be treated with hCG hormonal therapy monotherapy without concomitant recombinant FSH
- Stimulates Sertoli cells
- Secretion
- Stimulated by (2):
- Estrogen
- Activin
- Inhibited by (1):
- Inhibin
- Thought to account for the relative secretory independence of FSH from GnRH secretion
- Stimulated by (2):
- Function:
- Activin
- Secreted by Leydig cells
- Inhibin-B
- Secreted by Sertoli cells
- Production is stimulated by FSH
- Acts by negative feedback at the pituitary [Campbell’s 12th edition, page 1319 says both “hypothalamus or pituitary”, Wikipedia says “Inhibin does not inhibit the secretion of GnRH from the hypothalamus", 2019 AUA Update on Exogenous Testosterone and Male Reproduction agrees with Wikipedia] to inhibit FSH production
- Inhibin and activin can influence steroid production by Leydig cells
- Prolactin
- Normal levels may increase concentration of LH receptors on Leydig cells and sustain normal, high intratesticular testosterone levels
- May also potentiate the effects of androgens on growth and secretions of male accessory sex glands
- Hyperprolactinemia abolishes GnRH pulsatility and is a cause of infertility
Testis
- See Testis Anatomy Notes
- After binding LH, Leydig cells transport cholesterol into mitochondria and produce testosterone.