Inguinal Node Dissection: Difference between revisions
Jump to navigation
Jump to search
Urology4all (talk | contribs) |
Urology4all (talk | contribs) |
||
| Line 91: | Line 91: | ||
=== Technique === | === Technique === | ||
* See Surgical atlas. Surgical management of penile carcinoma: the inguinal nodes | * See [https://pubmed.ncbi.nlm.nih.gov/16643509/ Surgical atlas. Surgical management of penile carcinoma: the inguinal nodes] | ||
* '''<span style="color:#ff0000">Radical inguinal lymphadenectomy</span>''' | * '''<span style="color:#ff0000">Radical inguinal lymphadenectomy</span>''' | ||
** '''<span style="color:#ff0000">Boundaries of dissection:</span>'''§ | ** '''<span style="color:#ff0000">Boundaries of dissection:</span>'''[https://pubmed.ncbi.nlm.nih.gov/16643509/ §] | ||
*** '''<span style="color:#ff0000">Superior: inguinal ligament</span>''' | *** '''<span style="color:#ff0000">Superior: inguinal ligament</span>''' | ||
*** '''<span style="color:#ff0000">Medial: adductor longus muscle</span>''' | *** '''<span style="color:#ff0000">Medial: adductor longus muscle</span>''' | ||
Revision as of 13:18, 9 November 2022
See Contemporary management of patients with penile cancer and lymph node metastasis (Nat Rev Urol 2007)
Anatomic Considerations
Femoral Triangle
Borders
- Roof: fascia lata (covers femoral sheath)
- Floor: pectineus, iliopsoas, adductor longus muscles
- Superior: inguinal ligament (runs from anterior superior iliac spine to pubic tubercle)
- Lateral: medial border of sartorius muscle
- Medial: medial border of adductor longus muscle
Contents
Lateral to medial: NAVEL
- Nerve
- Artery
- Vein
- Empty space
- Allows the veins and lymph vessels to distend to accommodate different levels of flow
- Lymph nodes
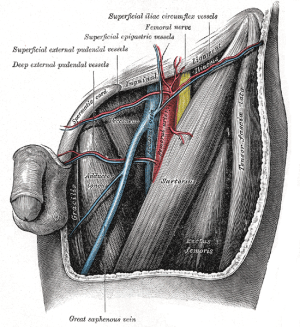
Nerves
- Femoral nerve
- Lies deep to the iliacus fascia
- Lateral to common femoral artery
- Functions
- Motor: innervates the pectineus, quadriceps femoris, and sartorius muscles
- Sensory: anterior thigh
- Should be preserved during inguinal dissection.
- Some of the sensory branches, however, are commonly sacrificed in the regional node dissection.
Vasculature
- Common femoral artery
- Divides into superficial femoral artery and deep (profunda) femoral artery
- Blood supply to the skin of the inguinal region is from branches of the common femoral artery. Complete inguinal dissection necessitates ligation of these branches.
- Viability of the skin flaps raised during the dissection depends on anastomotic vessels in the superficial fatty layer of the Camper fascia
- Medial to femoral nerve
- Common femoral vein
- Deep femoral vein and Great saphenous vein empty into the common femoral vein
- Medial to common femoral artery
Inguinal Lymph Nodes
- Classified as superficial vs. deep inguinal nodes
- Fascia lata of the thigh separates the superficial and deep inguinal nodes
- Superficial inguinal nodes
- Anatomic groups (5):
- Central nodes around the saphenofemoral junction
- Superolateral nodes around the superficial circumflex vein
- Inferolateral nodes around the lateral femoral cutaneous and superficial circumflex veins
- Superomedial nodes around the superficial external pudendal and superficial epigastric veins
- Inferomedial nodes around the greater saphenous vein
- Anatomic groups (5):
- Deep inguinal nodes
- Fewer in number, compared to superficial inguinal nodes
- Lie primarily medial to the femoral vein in the femoral canal
- Most cephalad of the deep inguinal nodes is the Node of Cloquet
- Node of Cloquet is located between the femoral vein and the lacunar ligament
- Lacunar ligament connects the inguinal ligament to the pectineal ligament
- Node of Cloquet is located between the femoral vein and the lacunar ligament
Penile Lymphatics
- Superficial lymphatic system
- Drains the prepuce and skin of the penile shaft
- Empties into the right and left superficial inguinal nodes
- Deep lymphatic system
- Drains the glans penis
- Empties into the superficial inguinal nodes and the deep inguinal nodes
- Penile cancer can metastasize to the contralateral inguinal nodes because of crossover in the symphyseal region
- Drainage subsequently proceeds from the inguinal nodes to the ipsilateral pelvic lymph nodes
- If the tumor has spread to the pelvic nodes, long-term survival is < 10%
- Lymphatic drainage of the penis to the groin runs beneath the Camper fascia
- Camper’s fascia can be preserved and left attached to the overlying skin when the superior and inferior skin flaps are fashioned. On the basis of this anatomy, a transverse skin incision least compromises this blood supply.
Inguinal Lymphadenectomy
- In the standard radical inguinal lymphadenectomy, both the superficial and deep inguinal lymph nodes are removed
- Superficial dissection removes nodes superficial to the fascia lata
Indications
- Clinically node-positive disease (palpable on physical exam)
- Clinically node-negative disease (not palpable on physical exam) but increased risk for inguinal metastasis based on primary tumor characteristics (pT ≥2, presence of vascular or lymphatic invasion, or grade ≥3).
- cN3 (fixed nodal mass) is managed initially with neoadjuvant chemotherapy followed by radical inguinal lymphadenectomy in responders
- May be curative when the disease is limited to the inguinal nodes.
Technique
- See Surgical atlas. Surgical management of penile carcinoma: the inguinal nodes
- Radical inguinal lymphadenectomy
- Boundaries of dissection:§
- Superior: inguinal ligament
- Medial: adductor longus muscle
- Lateral: sartorious muscle (saphenous vein and femoral vein in modified template)
- Inferior: apex of the femoral triangle/fossa ovalis (where the saphenous penetrates the fascia lata)
- Position: involved thigh slightly abducted and externally rotated with cushioned support under the flexed knee.
- Incision
- The inguinofemoral dissection is designed to cover an area outlined superiorly by a line drawn from the superior margin of the external ring to the anterior superior iliac spine, laterally by a line drawn from the anterior superior iliac spine extending 20 cm inferiorly, and medially by a line drawn from the pubic tubercle 15 cm down the medial thigh.
- In most situations the procedure is carried out through an oblique incision approximately 3 cm below and parallel to the inguinal ligament and extending from the lateral to the medial limit of the dissection (Fig. 39-21).
- If an area of the skin overlying the cancer-bearing nodes is invaded or adherent and requires excision, an elliptical incision is made around the involved skin and then extended medially and laterally. In this setting, the incision may alternatively be extended superiorly from the lateral border of the ellipse and inferiorly from the medial border to make a single S-shaped incision for the iliac and inguinofemoral dissections
- Superior and inferior skin flaps are developed in the plane just below the Scarpa fascia.
- The superior flap is elevated cephalad to a point 4 cm above the inguinal ligament, and the inferior flap to the limit of the dissection.
- The fat and areolar tissues are dissected from the external oblique aponeurosis and the spermatic cord to the inferior border of the inguinal ligament, forming the superior boundary of the lymph node packet
- The inferior angle of the inguinofemoral exposure is at the apex of the femoral triangle, where the long saphenous vein is identified and divided.
- In patients with minimal metastatic disease, it may be feasible and beneficial to spare the saphenous vein, and this should be considered to attempt to decrease the risk of lower-extremity complications.
- Dissection is deepened through the fascia lata overlying the sartorius muscle laterally and the thinner fascia covering the adductor longus muscle medially. At the apex of the femoral triangle, the femoral artery and vein are identified, and dissection is continued superiorly along the femoral vessels. Superficial cutaneous perforating arteries are ligated as they are encountered on the surface of the femoral artery. The saphenous vein is divided at the saphenofemoral junction, and the dissection is continued superiorly to include the deep inguinal nodes medial and lateral to the femoral vein until continuity with the pelvic dissection is attained at the femoral canal
- The anterior aspects of the femoral vessels are dissected, but the femoral vessels are not skeletonized, and the lateral surface of the femoral artery is not exposed.
- This avoids injury to the femoral nerve and the profunda femoris artery
- The femoral nerve is usually not visible as it runs beneath the iliacus fascia lateral to the femoral artery.
- This avoids injury to the femoral nerve and the profunda femoris artery
- After the femoral triangle is dissected the sartorius muscle is mobilized from its origin at the anterior superior iliac spine and either transposed or rolled 180 degrees medially to cover the femoral vessels.
- The muscle is sutured to the inguinal ligament superiorly, and its margins are sutured to the muscles of the thigh immediately adjacent to the femoral vessels
- The femoral canal is closed, if necessary, by suturing the shelving edge of the Poupart ligament to the Cooper ligament, being careful not to compromise the lumen of the external iliac vein or to injure the inferior epigastric vessels in the process.
- Closure
- Primary closure of the inguinofemoral dissection is usually possible with minimal or no further mobilization of the excision margins.
- When circumstances demand a large area of inguinal soft tissue sacrifice, primary closure may be obtained by scrotal skin rotation flaps an abdominal wall advancement flap or a myocutaneous flap based on the rectus abdominis or tensor fasciae latae for more extensive defects.
- Closed-suction drains are placed under the subcutaneous tissue and brought out inferiorly.
- During closure, the skin flaps are sutured to the surface of the exposed musculature to decrease dead space.
- The skin is closed with absorbable subcutaneous sutures and staples.
- Post-operative care
- The patient is maintained on bed rest for 2 or 3 days, and pneumatic compression stockings are used.
- Efforts to minimize lymphedema during the initial postoperative period include applying thigh-high elastic wraps or stockings and elevating the foot of the bed.
- The drains are removed after 5 to 7 days, when drainage is less than 30 to 40 mL/day.
- We maintain the patient on a suppressive dose of a cephalosporin for 1 to 2 months until healed to decrease the incidence of erythema and cellulitis, and this seems to improve overall wound healing.
- Adverse events:
- Hemorrhage
- Seroma or lymphocele
- Lymphedema, debilitating lymphedema
- Wound infection ornecrosis
- Flap necrosis
- DVT
- Sepsis
- Strong risk factor for complications is palliative indication for ILND§
- Boundaries of dissection:§
Modified complete inguinal lymphadenectomy
- Less morbidity than standard inguinal lymphadenectomy
- Key aspects of the procedure are (5):
- Shorter skin incision
- Limiting dissection by excluding the area lateral to the saphenous vein and femoral vein§
- Lateral limit of dissection saphenous and femoral vein in modified dissection
- Preservation of the saphenous vein
- Elimination of the need to transpose the sartorius muscle
- Thicker skin flaps
- Technique
- Position: frog-leg
- A 10-cm skin incision is made ≈1.5-2 cm below the inguinal crease
- Skin flaps are developed in the plane just beneath the Scarpa fascia for a distance of 8 cm superiorly and 6 cm inferiorly.
- The superior dissection is carried to the level of the external oblique fascia with exposure of the spermatic cord. A funiculus of lymphofatty tissue, extending from the base of the penis to the superomedial portion of the lymph node packet, is ligated and divided.
- Dissection commences in a caudad direction with removal of the superficial and deep inguinal nodes
- The saphenous vein is identified and preserved, although a number of branches draining into it will need to be sacrificed.
- The nodal packet is dissected caudad to the level of the skin flap dissection, at which point the lymphatics are carefully ligated and the specimen is delivered from the operative field
- A closed-suction drain is placed, and the incision is closed in standard fashion
- Adverse events:
- Primarily minor
- Seroma or lymphocele (0-26%)
- Lymphorrhea (9-10%)
- Wound infection and skin necrosis (0-15%)
- Primarily minor
Endoscopic and robotic inguinal lymphadenectomy
- The morbidity of an endoscopic inguinal lymph node dissection is lower than previously reported for open contemporary series with a similar number of nodes being harvested
Questions
- What part of the penis is drained by the superficial vs. deep lymphatic system?
- Which lymph nodes do the superficial vs. deep lymphatics of the penis drain to?
Answers
- What part of the penis is drained by the superficial vs. deep lymphatic system?
- Which lymph nodes do the superficial vs. deep lymphatics of the penis drain to?
References
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, vol 1, chap 39
- Leone, Andrew, et al. "Contemporary management of patients with penile cancer and lymph node metastasis." Nature Reviews Urology 14.6 (2017): 335-347.