Prostate: Difference between revisions
Jump to navigation
Jump to search
Urology4all (talk | contribs) |
Urology4all (talk | contribs) |
||
| Line 22: | Line 22: | ||
**# '''<span style="color:#ff0000">Transitional zone</span>''' | **# '''<span style="color:#ff0000">Transitional zone</span>''' | ||
**#* '''≈3-5% of the glandular prostate tissue''' | **#* '''≈3-5% of the glandular prostate tissue''' | ||
**#*In the young adult male, only constitutes about 5-10% of male prostate; with age and the development of BPH, the TZ can occupy a large part of the glandular prostate[https://www.baus.org.uk/_userfiles/pages/files/Publications/Transrectal%20Ultrasound%20%20Prostatic%20Biopsy%20FINAL.pdf] | |||
**#*Anterior to the peripheral zone | |||
**#* '''Separated''' </span>'''from the rest of the glandular compartments of the prostate by a distinct fibromuscular band</span>''' | **#* '''Separated''' </span>'''from the rest of the glandular compartments of the prostate by a distinct fibromuscular band</span>''' | ||
**#* '''<span style="color:#ff0000">Benign prostatic hyperplasia most commonly occurs in the transitional zone</span>''' | **#* '''<span style="color:#ff0000">Benign prostatic hyperplasia most commonly occurs in the transitional zone</span>''' | ||
Revision as of 17:02, 25 June 2023
Embryology
- Transitional and peripheral zone derived from urogenital sinus
- Central zone derived from Wollffian duct
- Homologous to the Skene glands in females
Gross Structure
- Ovoid in shape
- The base of the prostate is at the bladder-prostate junction
- The narrowed apex is the most inferior portion of the prostate gland, reaching the urogenital diaphragm. The apex of the prostate is continuous with the striated urethral sphincter
- The prostate is fixed to the pubic bone anteriorly by the puboprostatic ligaments near the apex of the prostate
- 70% of the prostate’s composition is glandular elements, 30% is fibromuscular stroma.
- The non-glandular anterior fibromuscular stroma is found extending from the bladder neck to the striated sphincter
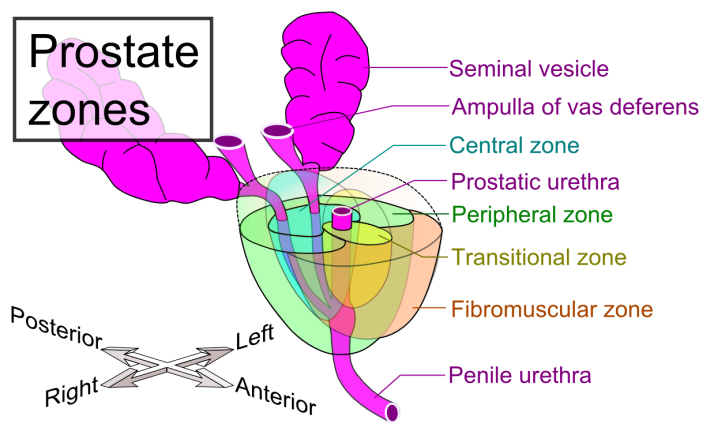
Mikael Häggström, M.D. Author info - Reusing images- Conflicts of interest: NoneMikael Häggström, M.D., CC0, via Wikimedia Commons - Glandular elements divided into 3 anatomic zones (largest to smallest):
- Peripheral zone
- ≈70% of the glandular prostate tissue
- Most (≈70%) prostate cancers occur in the peripheral zone
- Central zone
- ≈25% of the glandular prostate tissue
- Surrounds the opening of the ejaculatory ducts
- Transitional zone
- ≈3-5% of the glandular prostate tissue
- In the young adult male, only constitutes about 5-10% of male prostate; with age and the development of BPH, the TZ can occupy a large part of the glandular prostate[1]
- Anterior to the peripheral zone
- Separated from the rest of the glandular compartments of the prostate by a distinct fibromuscular band
- Benign prostatic hyperplasia most commonly occurs in the transitional zone
- ≈20% of prostate cancers occur in the transitional zone
- Peripheral zone
- The non-glandular anterior fibromuscular stroma is found extending from the bladder neck to the striated sphincter
Pelvic fasciae
- Fascial layers that surround prostate (3)§:
- Posteriorly: Denonvilliers fascia
- Anteriorly/anterolaterally: prostatic fascia (also inappropriately called the capsule of the prostate; recall no true histologic capsule)
- Laterally: prostatic fascia fuses with endopelvic fascia
- See Figures 1 and 2
- Denonvilliers fascia
- A filmy, delicate layer of connective tissue
- Located between the anterior wall of the rectum and prostate
- There is a plane of loose, areolar tissue between Denonvilliers fascia and the rectum
- Most prominent and dense near the base of the prostate and the seminal vesicles and thins dramatically as it extends caudally to its termination at the striated urethral sphincter
- Impossible to discern posterior and anterior layers of this fascia on microscopic examination; for this reason, this must be excised fascia completely to obtain an adequate surgical margin
- Prostatic fascia
- In direct continuity with the parenchyma of the prostate anteriorly and anterolaterally
- Fuses with the levator fascia laterally to form the lateral pelvic fascia
- Endopelvic fascia
- Also known as levator fascia, lateral prostatic fascia, and lateral pelvic fascia§
- Lines the inner surface of pelvic muscles
- Continuous with the transversalis fascia
- Denonvilliers fascia
- The cavernosal nerves (neurovascular bundles) travel between the levator/endopelvic and prostatic fascia, posterolateral to the prostate (See Figure 1, same as above)
Vasculature
Arterial Supply
- The blood supply to the prostate enters at the 4 and 8 o'clock positions.
- The prostate receives arterial blood supply from the inferior vesical artery, which is a branch of the anterior branch of the internal iliac artery
- After the inferior vesical artery provides small branches to the seminal vesicle and the base of the bladder and prostate, the artery terminates in 2 large groups of prostatic vessels:
- Urethral vessels
- Enter the prostate at the posterolateral vesicoprostatic junction and supply the vesical neck and periurethral portion of the gland.
- Capsular branches
- Run along the pelvic sidewall in the lateral pelvic fascia posterolateral to the prostate, providing branches that course ventrally and dorsally to supply the outer portion of the prostate.
- These capsular arteries and veins are intimately associated with the branches of the pelvic plexus forming the neurovascular bundle (NVB), which is used as the macroscopic landmark to aid in the identification of the microscopic branches of these nerves.
- Urethral vessels
- After the inferior vesical artery provides small branches to the seminal vesicle and the base of the bladder and prostate, the artery terminates in 2 large groups of prostatic vessels:
- Branches from the internal pudendal artery and the middle rectal (hemorrhoidal) artery also contribute a supply to the prostate
Venous Drainage
- The veins of the prostate drain into the Santorini/periprostatic plexus
- The periprostatic plexus anastomoses with the deep dorsal vein of the penis and the internal iliac (hypogastric) veins
- The deep dorsal vein leaves the penis under the Buck fascia between the corpora cavernosa and penetrates the urogenital diaphragm, with the common trunk dividing into 3 major branches:
- Superficial branch
- Right lateral venous plexuses
- Left lateral venous plexuses
- Superficial branch
- The centrally located vein overlying the bladder neck and prostate
- Lies in the retropubic fat outside the anterior prostatic fascia.
- Travels between the puboprostatic ligaments
- Easily visualized early in retropubic operations and has communicating branches over the bladder itself and into the endopelvic fascia.
- Right and left lateral venous plexuses
- Traverse posterolaterally
- Communicate freely with the pudendal, obturator, and vesical plexuses, which form the inferior vesical vein, which empties into the internal iliac vein.
- The common trunk (including deep dorsal vein complex) and lateral venous plexuses are covered by the prostatic and endopelvic/levator fascia.
- See Figure for representation of DVC in relationship to other surrounding veins
Lymphatic drainage
- The obturator and internal iliac nodes are the primary sites of drainage
- The presacral group or, infrequently, the external iliac nodes may receive a small portion of the initial lymphatic drainage.
- Limits of dissection for standard lymphadenectomy during radical prostatectomy:
- Superior: ureter/bifurcation of the common iliac artery
- Inferior: circumflex iliac vein and Cloquet’s node/Cooper ligament at the femoral canal
- Lateral: pelvic side wall (below external iliac vein)
- Medial: bladder
- Posterior: obturator nerve/fossa (internal iliac vein in extended PLND)
Nerve Supply
- In males, the pelvic plexus is located retroperitoneally beside the rectum 5 to 11 cm from the anal verge
- The nerves innervating the prostate travel outside the fascia of the prostate and Denonvilliers fascia until they perforate the fascia where they enter the prostate
Efferent
- Cavernous nerves
- From the pelvic plexus
- Provide sympathetic and parasympathetic innervation to the prostate
- Sympathetic fibers innervate the smooth muscle of the capsule and stroma for contraction.
- Parasympathetic fibers promote secretory function by terminating in the acini
- Pass by the tips of the seminal vesicles and course very close to the apex of the prostate, where they are most vulnerable to injury.
Affarent
- The pelvic plexuses carry afferent neurons from the prostate to the pelvic and thoracolumbar spinal centers
Imaging
Transrectal ultrasound
- TRUS uses probes with frequency ranging from 6-8 MHz
- Prostate volume can be calculated using an ellipsoid formula where volume = π/6 x L x W x H (0.52) (some use spheroid formula where volume = 4/3 x π × length × width × height or "bullet" formula described with volume calculator); this is accurate to within 5% of its true weight
MRI
- Zonal anatomy is best demonstrated by T2-weighted image
Questions
- From which zone of the prostate does the majority of prostate cancer arise from? BPH arise from?
- Which zone of the prostate surrounds the ejaculatory ducts? Which is the smallest zone?
- What are the primary lymphatic drainage sites of the prostate?
Answers
- From which zone of the prostate does the majority of prostate cancer arise from? BPH arise from?
- Prostate cancer usually (70%) arise from the peripheral zone; 20% arise in transitional zone
- BPH usually arises from the transitional zone
- Which zone of the prostate surrounds the ejaculatory ducts? Which is the smallest zone?
- Central zone
- Transitional zone
- What are the primary lymphatic drainage sites of the prostate?
- Obturator, internal iliac
References
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 21