Anatomy: Groin and Inguinal
Femoral Triangle
Borders
- Roof: fascia lata (covers femoral sheath)
- Fascia lata is continuous with external oblique aponeurosis superiorly[1]
- Floor: pectineus, iliopsoas, adductor longus muscles
- Superior: inguinal ligament (runs from anterior superior iliac spine to pubic tubercle)
- Inguinal ligament is the portion of the external oblique aponeurosis which extends between the anterior superior iliac spine and the pubic tubercle as a thick band, folded inward[2]
- Lateral: medial border of sartorius muscle
- Medial: medial border of adductor longus muscle
Contents
Lateral to medial: NAVEL
- Nerve
- Artery
- Vein
- Empty space
- Allows the veins and lymph vessels to distend to accommodate different levels of flow
- Lymph nodes
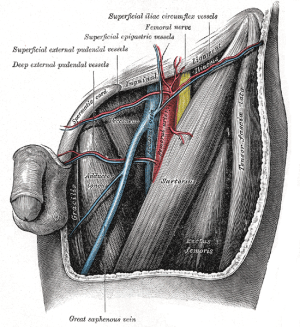
Nerves
- Femoral nerve
- Lies deep to the iliacus fascia
- Lateral to common femoral artery
- Functions
- Motor: innervates the pectineus, quadriceps femoris, and sartorius muscles
- Sensory: anterior thigh
- Should be preserved during inguinal dissection.
- Some of the sensory branches, however, are commonly sacrificed in the regional node dissection.
Vasculature
- Posterior to fascia lata
- Common femoral artery
- Continuation of external iliac artery
- External iliac artery above inguinal ligament, common femoral artery below inguinal ligament
- Gives off a branch called deep (profunda) femoral artery and continues as superficial femoral artery[3]
- Blood supply to the skin of the inguinal region is from branches of the common femoral artery.
- Complete inguinal dissection necessitates ligation of these branches.
- Viability of the skin flaps raised during the dissection depends on anastomotic vessels in the superficial fatty layer of the Camper fascia
- A transverse skin incision least compromises blood supply to the skin.
- Complete inguinal dissection necessitates ligation of these branches.
- Medial to femoral nerve
- Just medial to the midpoint of the inguinal ligament in the inguinal crease region[4]
- Continuation of external iliac artery
- Common femoral vein
- Deep femoral vein and Great saphenous vein (also known as long saphenous vein) empty into the common femoral vein
- Great saphenous vein approaches common femoral vein medially
- Deep femoral vein approaches common femoral vein laterally
- Medial to common femoral artery
- Deep femoral vein and Great saphenous vein (also known as long saphenous vein) empty into the common femoral vein
- Common femoral artery and common femoral vein are enclosed in femoral sheath[5]
Inguinal Lymph Nodes
- Classified as superficial vs. deep inguinal nodes
- Fascia lata of the thigh separates the superficial and deep inguinal nodes
- Superficial inguinal nodes
- Anatomic groups (5):
- Central nodes around the saphenofemoral junction
- Superolateral nodes around the superficial circumflex vein
- Inferolateral nodes around the lateral femoral cutaneous and superficial circumflex veins
- Superomedial nodes around the superficial external pudendal and superficial epigastric veins
- Inferomedial nodes around the greater saphenous vein
- Anatomic groups (5):
- Deep inguinal nodes
- Fewer in number, compared to superficial inguinal nodes
- Lie primarily medial to the femoral vein in the femoral canal
- Most cephalad of the deep inguinal nodes is the Node of Cloquet
- Node of Cloquet is located between the femoral vein and the lacunar ligament
- Lacunar ligament connects the inguinal ligament to the pectineal ligament
- Node of Cloquet is located between the femoral vein and the lacunar ligament
Penile Lymphatics
- Superficial lymphatic system
- Drains the prepuce and skin of the penile shaft
- Empties into the right and left superficial inguinal nodes
- Deep lymphatic system
- Drains the glans penis
- Empties into the superficial inguinal nodes and the deep inguinal nodes
- Primary site of metastatic spread of penile carcinoma occurs via the regional lymphatic system, first to the inguinal lymph node chain and then to the iliac and pelvic lymph nodes.
- Presence and extent of regional LN metastases is the single most important prognostic factor in determining the long-term survival of patients with penile cancer
- If cancer has spread to the pelvic nodes, long-term survival is < 10%
- Presence and extent of regional LN metastases is the single most important prognostic factor in determining the long-term survival of patients with penile cancer
- Inguinal metastatic spread can be unilateral or bilateral, and crossover drainage from the right to left groin or vice versa can also occur.
- Metastatic spread from the inguinal lymph nodes to the contralateral pelvis or from the right to left pelvis has never been reported.
- Skip lesions with direct lymphatic drainage from penile tumors to the pelvic lymph nodes has never been reported. .
- Further spread from the true pelvis to the retroperitoneal lymph nodes is beyond the regional drainage system of the penis and represents systemic metastatic disease