Spermatogenesis
Germ Cell Types[edit | edit source]
- 13 recognizable germ cell types:
- Dark type A spermatogonia (Ad)
- Pale type A spermatogonia (Ap)
- Type B spermatogonia (B)
- Preleptotene primary spermatocytes (R)
- Leptotene primary spermatocytes (L)
- Zygotene primary spermatocytes (Z)
- Pachytene primary spermatocytes (P)
- Secondary spermatocytes (II)
- Sa, Sb, Sc, Sd1, Sd2 spermatids
- Type A spermatogonia are the only true stem cell in the testis because they can either self-renew or differentiate to become sperm
- Total time to produce an ejaculated sperm ranges from 42 to 76 days, the majority of which is spent in the testicle
- Sperm spend 45 to 60 days developing in the testis and 2 to 12 days in the epididymis. They are not routinely found in the seminal vesicle, and spend only seconds in the ejaculatory ducts and urethra during ejaculation.
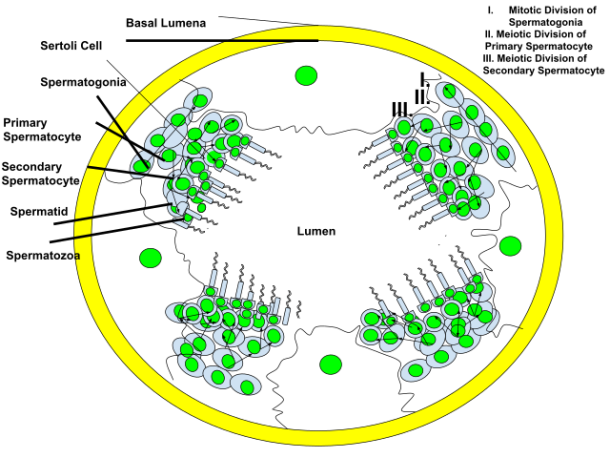
Phases of Spermatogenesis (3):[edit | edit source]
- Proliferative
- Spermatogonia divide to replace their number, or differentiate into daughter cells that become mature gametes
- Meiotic
- Crossing over of sister chromatids, exchange of genetic material, creation of unique daughter cells, and halving the number of chromosomes.
- Haploid gametes differ genetically from their adult precursors.
- Only occurs in gametes
- Mature primary spermatocytes are the first germ cells to undergo meiosis
- Faulty recombination can cause azoospermia and infertility
- The final product of meiosis is the spermatid
- Somatic cells replicate by mitosis, producing genetically identical daughter cells
- Mature primary spermatocytes are the first germ cells to undergo meiosis
- Only occurs in gametes
- Haploid gametes differ genetically from their adult precursors.
- Crossing over of sister chromatids, exchange of genetic material, creation of unique daughter cells, and halving the number of chromosomes.
- Spermiogenesis:
- Cellular remodeling and nuclear compaction of spermatid DNA; spermatids mature to become spermatozoa
- SpermatOGONIA (least differentiated) --› spermatOCYTE --› spermatID (most differentiated) --› spermatOZOA
Epididymis[edit | edit source]
- See Epididymis Anatomy Chapter Notes
- Functions (3):
- Sperm transport
- The principal mechanism responsible for moving spermatozoa through the epididymis is probably the spontaneous rhythmic contractions of the contractile cells surrounding the epididymal duct
- Sperm storage
- After migration through the caput (head) and corpus (body) of the epididymis, spermatozoa are retained in the cauda (tail) epididymis for varying lengths of time, depending on the degree of sexual activity
- Maturation of spermatozoa
- Maturation changes (4):
- Improving cell membrane structural integrity
- Increasing fertilization ability
- Improving motility
- Increased capacity for glycolysis
- Sperm fertility maturation in humans is, in most part, achieved at the level of the distal corpus (body) or proximal cauda (tail) epididymis
- Clinical implication: in men with congenital absence of the vas deferens or epididymal obstruction from vasectomy, sperm retreival should target the cauda (tail) for better sperm motlity compared to the caput (head)
- Maturation changes (4):
- Function influenced by temperature
- Sperm transport
- Fate of unejaculated sperm unknown
- Testosterone and DHT are in high concentration
Vas Deferens[edit | edit source]
- See Vas Deferens Anatomy Chapter Notes
- Functions
- Has both absorptive and secretory functions
- Actively converts testosterone to DHT
- Does not store sperm
- Immediately before emission, with sympathetic stimulation, sperm is rapidly transported from the distal epididymis through the vas deferens to the ejaculatory duct
- After ejaculation, the contents of the vas deferens are propelled back into the epididymis
Seminal vesicles[edit | edit source]
- Secrete 70-80% of ejaculatory fluid, with the remainder coming from the prostate, vas deferens, and periurethral Cowper glands
- Seminal fluid
- Contains fructose
- Functions:
- Coagulates semen
- Promotes sperm motility
- Increases stability of sperm chromatin
- Suppresses immune activity in the female reproductive tract
- Provides anti-oxidant protection to sperm
- Alkaline pH
- Mixing of alkaline seminal vesicle with acidic prostatic secretions results in human semen having a mildly alkaline pH
- Clinical implication: acidic ejaculate (pH<7.2) is associated with blockage or absence of seminal vesicles
- Mixing of alkaline seminal vesicle with acidic prostatic secretions results in human semen having a mildly alkaline pH
Spermatozoa[edit | edit source]
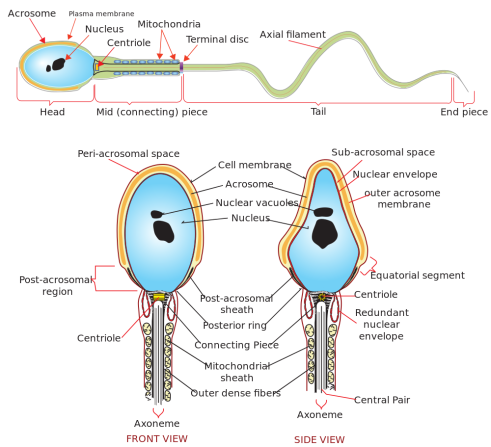
- Morphologic sections (3):
- Head (contains a nucleus and an acrosome)
- Acrosome is needed for fertilization (specifically, capacitation)
- Lack of acrosome is associated with round-headed sperm
- Clinical implication: round-headed sperm morphology is associated with infertility
- Neck (connecting piece and proximal centriole)
- Tail (midpiece, principal piece, endpiece)
- The Midpiece in the tail contains the Mitochondria
- Head (contains a nucleus and an acrosome)
- Ciliated cells with a 9+2 axonemal structure that allows motility
- Utilize glucose and fructose (from seminal vesicles) for energy
- Processes that must occur for a sperm to normally fertilize an egg include (4):
- Development of motility
- Acrosome reaction
- Capacitation
- Zona pellucida binding
Aging[edit | edit source]
- Testosterone decrease with age, causes are multifactorial:
- Fewer Leydig cells
- More testosterone-binding proteins, including SHBG, resulting in decreased bioavailable testosterone
- Loss of diurnal variation of testosterone secretion
- Blunted HPG feedback response to low testosterone (despite generally high levels of gonadotropins) and to GnRH stimulation
- Irregular GnRH pulses that are less effective in stimulating gonadotropin release
- FSH levels increase with age
- Sperm production decrease with age
- An age-related decrease in sperm production in older testes appears to stem from decreased germ cell proliferation, rather than increased cellular degeneration
- Increasing paternal age increases the fraction of sperm with sex chromosomal aneuploidies. However, little evidence to support a paternal age-related increase in aneuploid births, except possibly trisomy 21 and disomy 1
Questions[edit | edit source]
- What hormones are secreted by the anterior pituitary?
Answers[edit | edit source]
- What hormones are secreted by the anterior pituitary?
Next Chapter: Epidemiology and Etiology of Infertility[edit | edit source]
References[edit | edit source]
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 22
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 23
- Rambhatla A, Mills JN. 2017 AUA Update on Primary, Secondary and Adult Onset Hypogonadism: Diagnosis and Treatment