Penis and Urethra Surgery
INCLUDES PARTS of CUAJ 2019 Penile Lesions Review
Principles of Reconstructive Surgery
Graft vs. Flap
- Tissues can be transferred as a graft or flap
- The term flap implies that the tissue is excised and transferred WITH THE BLOOD SUPPLY either preserved or surgically re-established at the recipient site
- Important considerations for the use of flaps in urethral reconstruction:
- Nature of the flap tissue
- Vasculature of the flap
- Mechanics of flap transfer
- Important considerations for the use of flaps in urethral reconstruction:
- The term graft implies that tissue is excised and transferred to a graft host bed, where a NEW BLOOD SUPPLY develops by a process termed take
- Take requires ≈96 hours and occurs in 2 phases:
- Initial phase: imbibition
- Requires ≈48 hours
- Graft survives by “drinking” nutrients from the adjacent graft host bed
- Temperature of the graft is less than the core body temperature
- Second phase: inosculation
- Requires ≈48 hours
- True microcirculation is reestablished in the graft
- Temperature of the graft increases to core body temperature
- Initial phase: imbibition
- Take requires ≈96 hours and occurs in 2 phases:
Tissue Grafts
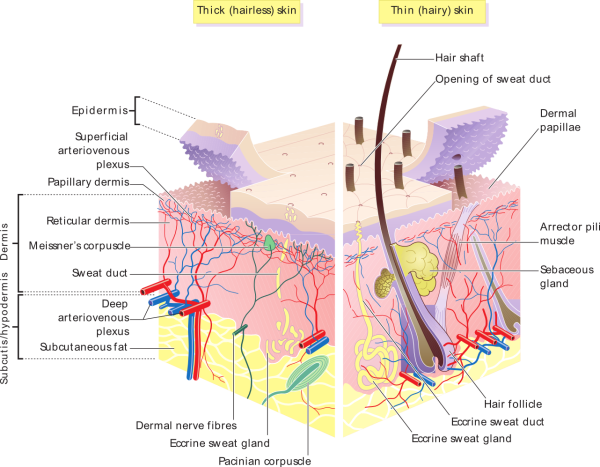
Graft Anatomy
- Superficial to deep:
- Epidermal, or epithelial layer
- Acts as the barrier to the “outside”
- Superficial dermis, or superficial lamina or papillary dermis
- Deep dermis, or deep lamina or reticular dermis
- On the undersurface of the deep dermal layer or deep lamina is the deep plexus.
- In the case of skin, this deep plexus is called the subdermal plexus
- Contains most of the lymphatics
- Greater collagen content than found in the superficial dermal layer
- Generally thought to account for the physical characteristics of the tissue
- On the undersurface of the deep dermal layer or deep lamina is the deep plexus.
Classification
- Split-thickness vs. full-thickness
Split-thickness graft
- Carries the epidermis (or the covering) and variable amount of [superficial] dermis
- Reticular dermis is not carried with the split-thickness skin graft
- Exposes the superficial dermal (intradermal or intralaminar) plexus
- Advantage:
- Favorable vascular characteristics
- Disadvantage:
- Tends to contract and be brittle when mature
- A mesh graft is usually an application of the split-thickness graft.
- After the harvest of a sheet graft, the sheet is placed on a carrier that cuts systematically placed slits in the graft. These slits can expand the graft by various ratios.
- For most genital reconstructive surgery, the slits are not for expansion but rather to allow subgraft collections to escape and allow the graft to conform better to irregular graft host beds (e.g., the testes in split-thickness skin graft scrotal construction).
- After the harvest of a sheet graft, the sheet is placed on a carrier that cuts systematically placed slits in the graft. These slits can expand the graft by various ratios.
Full-thickness graft
- Carries the epidermis (or the covering) and all of the dermis (the superficial dermis (or lamina) and the deep/reticular dermis (or deep lamina)).
- Exposes the subdermal plexus in skin.
- A full-thickness unit carries most of the lymphatics, and the physical characteristics are likewise carried with the transferred tissue
- Advantage:
- Does not contract as much and is more durable when mature
- Disadvantage:
- More fastidious vascular characteristics
Grafts in Urology
Primary urethral reconstruction (5)
- Oral mucosal graft
- Can be taken from the cheek (buccal), the lip (labial), and the undersurface of the tongue (lingual);
- Buccal mucosa is thought to have a panlaminar plexus
- Skin grafts (full-thickness (FTSG) and split-thickness (STSG))
- STSGs have been used for staged anterior urethral reconstruction
- Extragenital FTSGs have an increased mass compared to genital FTSGs.
- This increased mass makes the graft more fastidious, and the poor results reported with urethral reconstruction with extragenital FTSGs are probably due to poor or ischemic take.
- The posterior auricular graft (Wolfe graft) is an exception to the rule concerning extragenital skin.
- Skin island flaps based on the dartos fascia or tunica dartos
- Rectal mucosa graft
- Little is known about the characteristics of the rectal mucosal graft
- Bladder epithelial graft
- Issues with desiccation and hypertrophic growth have limited its use in the distal urethra
- The bladder epithelial graft and the oral mucosal graft have numerous vascular properties that make them desirable for urethral reconstruction.
- Tunica vaginalis grafts have been tried for urethral reconstruction with uniformly poor results.
Penile reconstruction
- STSGs (preferred) and FTSGs and have been used for penile reconstruction.
- The highest probability of 100% graft take and best cosmetic results occur with penile skin reconstruction using an unmeshed thick (0.012 - 0.015 inch) STSG.
- Meshed or thinner STSGs have more of a tendency to contract which compromises penile functionality and cosmesis.
- FTSGs may provide adequate cosmesis but are associated with a higher incidence of failure of the graft to take.
- The results with STSGs are so good that FTFGs are rarely used for coverage of the penis.
- Local skin flaps from the abdomen or thigh generally do not produce the same cosmetic outcomes.
- The highest probability of 100% graft take and best cosmetic results occur with penile skin reconstruction using an unmeshed thick (0.012 - 0.015 inch) STSG.
- Tunica vaginalis grafts have proved useful for small defects of the tunica albuginea of the corpora cavernosa.
Generalities of reconstructive surgical techniques
- Reconstructive surgery is performed with all efforts aimed at minimizing tissue injury and promoting healing.
- Bipolar surgery is often preferred.
- With cautery, the electrical charge is grounded either to a pad (monopolar) or to the opposite tong of the forceps (bipolar).
- Because electricity is dissipated by conductors (in the case of human tissue, vessels, and nerves), there is a possibility of damage to these delicate structures.
- In most instances, the field effects of the electricity are more confined with bipolar cautery.
- In urethral surgery, absorbable suture is the rule. The needle should be tapered if possible
- Femoral neuropathy can occur after lithotomy procedures due to hip hyperabduction/hyperextension, or secondary to retractor injury with abdominal/pelvic procedures.
- The femoral nerve, the largest branch of the lumbar plexus, is formed within the psoas muscle from the fusion of the anterior divisions of L2-L4. It emerges between the psoas major and iliacus muscles just superior to the inguinal ligament and enters the thigh lateral to the external iliac artery.
- Sensory branches are the anterior and medial femoral cutaneous and long saphenous nerves.
- Responsible for sensation of anterior thigh and medial leg
- Motor supply is to the psoas, iliacus, quadriceps, pectineus, and sartorius muscles.
- Responsible for knee extension.
- Sensory branches are the anterior and medial femoral cutaneous and long saphenous nerves.
- The femoral nerve, the largest branch of the lumbar plexus, is formed within the psoas muscle from the fusion of the anterior divisions of L2-L4. It emerges between the psoas major and iliacus muscles just superior to the inguinal ligament and enters the thigh lateral to the external iliac artery.
Urethral stricture disease
- See AUA Urethral Stricture Guideline Notes
- If a normal urethra measures 30 Fr, its outer diameter is 10 mm
- "Urethral stricture" refers to anterior urethral disease
- The term urethral stricture describes a process that involves the urethral epithelium along with the spongy erectile tissue of the corpus spongiosum, and this is referred to as spongiofibrosis.
- The anterior urethra is surrounded by corpus spongiosum
- The posterior urethra is NOT surrounded by corpus spongiosum
- Narrowing of the posterior urethra is not referred to as a stricture. Obliterative processes of the membranous urethra, such as those associated with pelvic fracture, would be referred to as pelvic fracture urethral injury (PFUI), and other narrowing processes of the posterior urethra are correctly referred to as either contractures or stenoses.
- Contraction and non-compliance of the scar reduces the urethral lumen.
- The term urethral stricture describes a process that involves the urethral epithelium along with the spongy erectile tissue of the corpus spongiosum, and this is referred to as spongiofibrosis.
- Squamous metaplasia is often seen involving the urothelium of the urethra proximal to a narrow caliber urethral stricture.
Causes
Acquired
- Trauma (most common cause in developing countries)
- Most urethral strictures are the result of straddle trauma
- This trauma often goes unrecognized until the patient presents with voiding symptoms resulting from the obstruction of the stricture or scar
- Iatrogenic trauma to the urethra still exists, but with the development of small endoscopes and the limitation of indications for cystoscopy in boys, we see fewer iatrogenic strictures today than in the past.
- Most urethral strictures are the result of straddle trauma
- LS-related urethral strictures
- Tend to be longer
- May have a higher association with urethral cancer
- Infection
- Inflammatory strictures associated with gonorrhea were the most commonly seen in the past and are less common now.
- With the advent of prompt and effective antibiotic treatment, gonococcal urethritis progresses less often to gonococcal urethral strictures.
- The role of Chlamydia and Ureaplasma urealyticum (i.e., nonspecific urethritis) in the development of anterior urethral strictures is unclear
- Inflammatory strictures associated with gonorrhea were the most commonly seen in the past and are less common now.
Congenital
- Criteria to define a congenital stricture:
- Not an inflammatory stricture
- Short-length stricture
- Not associated with a history of or potential for urethral trauma.
- These criteria limit the term congenital stricture to strictures of the anterior urethra found in infants before they attempt erect ambulation. So defined, congenital strictures are the rarest encountered
Idiopathic
- Most common cause in developed countries
Diagnosis and Evaluation
- For an appropriate treatment plan to be devised, it is important to determine the location, length, depth, and density of the stricture (spongiofibrosis).
- Length and location of the stricture can be determined using:
- Radiographs
- Urethroscopy
- Ultrasonography.
- Length and location of the stricture can be determined using:
History and Physical exam
- History
- Most often present with obstructive voiding symptoms or urinary tract infections such as prostatitis and epididymitis.
- Some patients also present with urinary retention.
- On close inquiry, most of these patients are found to have tolerated notable voiding symptoms for a long time before progressing to complete obstruction.
Imaging
- Retrograde urethrography/VCUG
- Ultrasound
- Most accurate method to determine the length of a graft needed for repair of an anterior urethral stricture.
- MRI
- Has been suggested as useful in patients with pelvic fracture urethral distraction, particularly in cases in which the anatomy of the pelvis has become significantly distorted.
- With regard to anterior urethral stricture, however, MRI has not been useful, with the exception of those cases in which there is urethral carcinoma.
Other
- Endoscopy
Management
Options (4):
- Dilation
- Direct Visual Internal Urethrotomy
- Urethral stent
- Urethroplasty
Dilation
- Goal of this treatment, a concept that is frequently forgotten, is to stretch the scar without producing more scarring.
- If bleeding occurs during dilation, the stricture has been torn rather than stretched, possibly further injuring the involved area.
- The practice of blind passage of filiforms and blind dilation without knowledge of the anatomy of the urethral stricture is condemned.
- Dilation can be curative and has short-term and mid-term efficacy rates equal to internal urethrotomy based on retrospective analysis, though there has been no RCT comparing the two.
Direct Visual Internal Urethrotomy (DVIU)
- Involves incision through the scar to healthy tissue to allow the scar to expand and the lumen to heal enlarged.
Technique
- Usually, a single incision is made at the 12 o’clock position.
- However, the 12 o'clock position might be questioned based on the location of the urethra within the corpus spongiosum.
- Although the anterior aspect of the corpus spongiosum is thicker, a deep incision in the more distal aspects of the anterior urethra will certainly enter the corpora cavernosa, and these incisions have been associated with the creation of erectile dysfunction.
- However, the 12 o'clock position might be questioned based on the location of the urethra within the corpus spongiosum.
- Normal saline should be used as the irrigant
- To date, the results of laser urethrotomy are mixed.
Adverse events
- Recurrence of stricture (most common complication).
- Studies have shown that the failure rate of long-term catheterization after internal urethrotomy is similar to that seen with 3-7 days of catheterization
- Bleeding (almost always associated with erections immediately after the procedure)
- Extravasation of irrigation fluid into the perispongiosal tissues
- Erectile dysfunction
- Decreased success rate of reconstruction
- Many studies have shown that the success of reconstruction is diminished by multiple prior urethral dilations and internal urethrotomy
Urethral stent
- Contraindications to the use of the UroLume:
- Prior substitution urethral reconstruction, particularly where skin has been incorporated into the urethra
- Contact of the stent with the skin is associated with a virulent hypertrophic reaction.
- Poor candidates for the UroLume includes patients with strictures associated with deep spongiofibrosis.
- Patients who fall into this category have had urethral distraction injuries and straddle injuries associated with deep fibrosis.
- Prior substitution urethral reconstruction, particularly where skin has been incorporated into the urethra
- Technique
- Must be placed only in the bulbar urethra
- When placed beyond the area of the scrotal urethra, placement has been associated with pain on sitting and intercourse.
- Some patients (particularly young patients) complain of perineal pain, often with vigorous activity, even after implantation of the stent in the deep bulbous urethra.
- Longer bulbous strictures require two stents that are overlapped. These stents can migrate away from each other, leaving a gap between them where recurrence of stricture is inevitable. When this occurs, the stricture recurrence is excised, and a third stent is placed to span the gap.
- UroLume has been taken off the market and is currently not available for implantation.
- Must be placed only in the bulbar urethra
- Adverse Events
- Permanently implantable stents, such as UroLume are associated with unique complications.
- However, there are still many patients who will present with UroLume stents, and many will need treatment.
Open reconstruction: excision and reanastamosis
Technique
- The best results are achieved when the following technical points are observed:
- The area of fibrosis is totally excised
- Urethral anastomosis is widely spatulated, creating a large ovoid anastomosis
- Anastomosis is tension free
- Steps to gain urethral length:
- Vigorous mobilization of the corpus spongiosum
- Development of the intracrural space and detachment of the bulbospongiosus from the perineal body
- When the length of stricture precludes total excision of fibrosis with primary anastomosis, tissue transfer in the form of graft or flap is required.
- Tubularized grafts and skin islands should be avoided, if possible.
- Onlay procedures (graft or flap) are associated with a higher success rate than tubularized grafts or tubularized skin islands.
- Excision with primary anastamosis should be avoided in patients with a history of hypospadias repair due to expected altered or absent retrograde blood supply to the urethra through the normal arborization in the glans
- Tubularized grafts and skin islands should be avoided, if possible.
- It is imperative to evaluate the urethra completely proximal and distal to the stricture with endoscopy and bougienage during surgery to ensure that all the involved urethra is included in the reconstruction.
Adverse Events
- Sexual dysfunction
- Permanent ejaculatory dysfunction
- May occur in as high as 20% of men following urethroplasty.
- Complaints are usually related to pooling of semen within the urethra and/or loss of force with ejaculation. The etiology is poorly defined but is presumed to be due to either tortuosity of the neourethra and/or dysfunction of the bulbocavernosal muscle.
- Temporary erectile dysfunction
- Found in up to 20% of individuals undergoing an anterior urethroplasty.
- This incidence is similar between all types of anterior urethroplasties, e.g., excision and primary anastomosis, vascularized or graft urethroplasties.
- The erectile dysfunction symptoms classically resolve 6 six months with < 3-4% of patients reporting a permanent alteration in their erectile capabilities.
- Overall, the rate of erectile dysfunction after urethroplasty was ≈equal to the rate after circumcision.
- Longer-segment reconstructions were associated with a higher risk of postoperative erectile dysfunction, although the patient’s erectile function improved over time in many cases.
- Found in up to 20% of individuals undergoing an anterior urethroplasty.
- New onset of penile curvature
- May occur usually following an overaggressive attempt at excision and primary anastomosis performed in the distal bulbar region.
- Loss of libido and anorgasmia
- Very rare and are predominately due to a psychological component.
- Permanent ejaculatory dysfunction
Pelvic fracture urethral injuries
- See AUA Urethral Stricture Guideline Notes
- PFUIs are the result of blunt pelvic trauma and accompany ≈10% of pelvic fracture injuries
- Although total disruption of the urethra is possible with a straddle injury, straddle injuries most commonly involve only the bulbar urethra
- Distraction injuries are unique to the membranous urethra
- The most frequent point of distraction is at the departure of the bulbous urethra from the membranous urethra
- Diagnosis and Evaluation
- Important to define the precise anatomy of the pelvic fracture injury before treatment is undertaken
- A cystogram outlines the bladder and provides information about rostral displacement of the proximal urethra.
- The appearance of the bladder neck on contrast studies or on antegrade endoscopy does not accurately predict the ultimate function of the bladder neck after urethral reconstruction
- In the past, great reliance was placed on whether the bladder neck was closed or open on cystography.
- Lack of contrast in the prostatic urethra would suggest a competent, closed bladder neck whereas contrast in the prostatic urethra would suggest an incompetent, open bladder neck
- A lack of contrast material in the posterior urethra gives some information, about the integrity of the bladder neck. However, contrast material may opacify the prostatic urethra when the bladder neck is more than adequately competent for continence
- Lack of contrast in the prostatic urethra would suggest a competent, closed bladder neck whereas contrast in the prostatic urethra would suggest an incompetent, open bladder neck
- In the past, great reliance was placed on whether the bladder neck was closed or open on cystography.
- The appearance of the bladder neck on contrast studies or on antegrade endoscopy does not accurately predict the ultimate function of the bladder neck after urethral reconstruction
- Repair
- In most cases, PFUIs are not long, and the resultant obliteration is amenable to a technically straightforward mobilization of the corpus spongiosum with a primary anastomotic technique.
- Aggressive mobilization of the corpus spongiosum is performed with caution, because it is thought to have possible ill effects on retrograde blood supply, which in the pelvic fracture patient may be tenuous.
- Meticulous detachment of the investment of Buck fascia from the corpus spongiosum increases the compliance of the corpus and limits the need for aggressive mobilization.
- Aggressive mobilization of the corpus spongiosum is performed with caution, because it is thought to have possible ill effects on retrograde blood supply, which in the pelvic fracture patient may be tenuous.
- Anastomosis of the proximal anterior urethra can be done to any segment of the posterior urethra (apical, prostatic, or below)
- Most PFUIs can be managed by the exaggerated lithotomy position for the perineal approach.
- The boots are positioned to avoid stretch injuries of the common peroneal nerves.
- The common peroneal [also called fibular] nerve is a nerve in the lower leg that provides sensation over the posterolateral part of the leg and the knee joint.
- It divides at the knee into two terminal branches: the superficial fibular nerve and deep fibular nerve, which innervate the muscles of the lateral and anterior compartments of the leg respectively.
- When the common peroneal nerve is damaged or compressed, foot drop can be the end result.
- The boots are positioned to avoid stretch injuries of the common peroneal nerves.
- Summary of Steps:
- After the patient is correctly positioned, the perineal approach to reconstruction begins with an incision and dissection anterior to the transverse perinei musculature (anterior perineal triangle). We use a λ-shaped incision that is carried sharply down to the midline fusion of the ischiocavernosus musculature, then beneath the scrotum, to expose the uninvested portion of the corpus spongiosum. We then place a self-retaining ring retractor. The fusion of the ischiocavernosus musculature is divided, and the musculature is cleanly dissected from the corpus spongiosum and bulbospongiosum. The corpus spongiosum is detached from the triangular ligament and corpora cavernosa, the bulbospongiosum is detached from the perineal body, and the dissection is carried farther down to the infrapubic space. Posterior detachment of the bulbospongiosum is carried anteriorly, and the dissection is eventually carried through the area of fibrosis. We divide the triangular ligament and vigorously develop the intracrural space down to the pubis. If the dorsal vein is encountered, it is ligated and divided. If a tension-free anastomosis is thought to be impossible, we mobilize the corpus spongiosum. The proximal urethrotomy is spatulated; 10 to 12 anastomotic sutures are placed. The anastomotic sutures are placed in their respective locations. Before seating the anastomosis, we introduce a soft silicone (Silastic) ribbed urethral stenting catheter through the anastomosis under direct vision. Next, we reattach the corpus spongiosum to the corpora cavernosa and the bulbospongiosum to the perineal body. We place a small suction drain deep to the closure
- In cases in which the proximal urethra is significantly distracted in a rostral direction, the surgeon must be prepared to perform:
- Mobilize corpus spongiosum
- Development of the intracrural space and detachment of the bulbospongiosus from the perineal body
- Sequesterectomy (removal of sequestrum (scar) associated with defect)
- Corporeal rerouting (re-route the urethra under one side of the corpus cavernosum)
- Infrapubectomy
- Potential long-term sequelae of pubectomy:
- Shortening of the penis
- Destabilization of erection
- Destabilization of the pelvis, resulting in a chronic pain syndrome with exercise
- Potential long-term sequelae of pubectomy:
- It is important to try to avoid the creation of chordee during the repair of a distraction injury.
- In most cases, PFUIs are not long, and the resultant obliteration is amenable to a technically straightforward mobilization of the corpus spongiosum with a primary anastomotic technique.
- Postoperative management
- Urine is diverted via the suprapubic cystostomy, and the small soft silicone (Silastic) urethral catheter is plugged and serves as a stent only.
- After the reconstruction, patients are initially kept at bed rest for 24-48 hours and then ambulated and discharged with the suprapubic catheter and stenting urethral catheter in place.
- Patients are discharged on a regimen of oxybutynin and a suppressive antibiotic only if the pre-operative urine culture was positive. The drains are removed as drainage allows.
- A voiding trial with contrast material is performed between 3-4 weeks post-operatively.
- The trial involves removing the urethral catheter, filling the patient’s bladder with contrast material, and instructing him to void.
- The voiding film is examined to ensure that there is no extravasation and that the anastomosis appears widely patent.
- A urine culture specimen is also obtained, and the suprapubic catheter is plugged.
- The patient is allowed to void through the urethra for 5-7 days, and the suprapubic catheter is then removed.
- ≈6 months postoperatively and again 1 year later, patients are evaluated with flexible endoscopy.
- With the use of the techniques discussed or similar techniques, curative rates for reconstruction of posterior PFUIs are in the high 90% range.
- In general, failures are indicative of ischemia of the proximal corpus spongiosum with ensuing stenosis of the mobilized corpus spongiosum.
- Duplex ultrasound has been used to predict the patients at risk for this ischemic atrophy phenomenon.
- Patients with an intact pudendal artery on one side often were potent and were reliably cured with reconstruction.
- Patients with only reconstituted vessels, either unilateral or bilateral, never were potent but were reliably reconstructed. We found that these patients were optimal candidates for penile arterial revascularization to improve potency.
- Patients do well with reconstruction if they have at least one side that is reconstituted, and the only patients at risk for ischemic stenosis are patients with bilateral complete obstruction of the internal pudendal vessels. In such patients, we perform penile arterial revascularization to augment the vascularity and, with that accomplished, proceed to urethral reconstruction
- Duplex ultrasound has been used to predict the patients at risk for this ischemic atrophy phenomenon.
- In general, failures are indicative of ischemia of the proximal corpus spongiosum with ensuing stenosis of the mobilized corpus spongiosum.
- In many cases of pelvic fracture urethral distraction defects, erectile dysfunction is a consequence of the injury, although erectile dysfunction clearly results from the reconstructive surgery in some patients.
Lichen sclerosis (LS)
- A chronic inflammatory hypomelanotic, lymphocyte-mediated skin disorder that predominately affects the genitalia and may involve the prepuce, glans penis, urethral meatus, and fossa navicularis
- Associated with urethral strictures in males
- Possible mechanisms include:
- Iatrogenic stricture resulting from repeated instrumentation
- Pressure voiding associated with meatal stenosis causing secondary intravasation of urine into the glans Littre
- In females, urethral stricture is not a common feature of LS
- Possible mechanisms include:
- Associated with urethral strictures in males
- Previously known as balanitis xerotica obliterans
- Epidemiology
- Affects primarily middle-aged men, but it can occur in boys
- Most common cause of meatal stenosis in the adult
- Meatal stenosis in the male child appears to be a consequence of circumcision, which allows for ammoniacal meatitis. Children seen with ammoniacal meatitis are usually started with meatal dilation using steroid cream. Within a week, the process seems to settle down.
- Presents mainly in uncircumcised men
- Most common cause of meatal stenosis in the adult
- Affects primarily middle-aged men, but it can occur in boys
- Risk factors
- Cause has not been defined.
- Many mechanisms have been proposed:
- Trauma
- Auto-immune
- Genetic
- Infection
- A study identified Borrelia burgdorferi infection in affected tissues in the early course of the disease§
- Patients are more likely to be active tobacco smokers, have a higher body mass index, hypertension, diabetes mellitus, coronary artery disease, and have longer urethral strictures compared to non-LS urethral strictures§
- Diagnosis and Evaluation
- History and Physical Exam
- History
- Signs and Symptoms§
- Skin itching
- Bleeding
- Penile skin scarring, adhesions to the glans
- Acquired buried penis
- Pain
- Dyspareunia
- Painful erections
- Signs and Symptoms§
- Physical exam
- Appears as a whitish plaque
- See Figure
- Other: biopsy
- Diagnosis is made through biopsy
- History
- History and Physical Exam
- Capable of malignant transformation, progressing to squamous cell carcinoma in 2-8% of patients
- 4–6% of patients with penile squamous cell carcinoma have associated LS
- Management
- Dermatologic management of genitalia
- Treatment of genital skin LS reduces symptoms and progression to extensive stricture of the penile urethra§
- 2023 AUA Urethral Stricture Guidelines§
- Topical moderate- to high-potency steroid creams, such as clobetasol or mometasone creams
- Calcineurin inhibitors such as tacrolimus have been shown to cause regression in external skin manifestations.
- CUA Penile Lesions 2019 Review: 0.05% clobetasol propionate (steroid) cream applied daily for 2–3 months
- Lichen sclerosis associated urethral stricture
- Strictures tend to be longer, compared to non-LS urethral strictures§
- Strictures are more likely to be located in the penile urethra§
- Urethroplasty is challenging in this population, often requires multiple oral mucosa grafts to reconstruct long-segment strictures, often with a lower success rate compared to non-LS urethral strictures§
- Most surgeons now believe that LS is a disease of genital skin. For this reason, genital skin is not appropriate for reconstruction in patients with LS.
- Although it is technically possible to use extragenital skin for reconstruction, oral mucosal grafting has emerged as a better tissue in patients with LS associated urethral strictures.
- Campbell’s:
- The combination of topical steroids and antibiotics may help stabilize the inflammatory process. Conservative therapy may be warranted in patients whose meatus can easily be maintained at 14 to 16 French. In these cases, intermittent catheterization with lubrication of the catheter and meatal dilator with 0.05% clobetasol (Temovate) may be adequate treatment. Long-term antibiotic therapy may also be helpful to improve inflammation because secondary infection of the inflamed tissue may occur.
- Surgery is indicated in young patients with severe meatal stenosis.
- Because patients with long-standing meatal stenosis often have severe proximal urethral stricture disease, retrograde urethrography should be performed before therapy is initiated.
- If only the foreskin is involved, circumcision may be curative
- Dermatologic management of genitalia
Vesicourethral distraction defects
- Pathogenesis
- Complication of radical prostatectomy.
- Diagnosis and Evaluation
- Important to determine the length of the defect accurately.
- Management
- An indwelling suprapubic tube must always be considered an option.
- Other options are endoscopic treatment, continent catheterizable bladder augmentation (may be a better operation than aggressive functional reconstruction), and diversion
Urethral hemangioma
- Rare condition that is usually persistent
- All reported cases of urethral hemangioma have been benign
- Management
- Depends on symptoms, size and location of the lesion
- Asymptomatic lesions do not require treatment and should be observed because hemangiomas can regress spontaneously.
- Symptomatic lesions that require treatment must be completely excised to prevent recurrence. Small lesions can be treated with laser, larger lesions are treated with open excision
- Depends on symptoms, size and location of the lesion
Reactive arthritis
- Characterized by a classic triad of:
- Arthritis
- Conjunctivitis
- Urethritis
- Urethral involvement is usually mild and self-limited and constitutes a minor portion of the disease.
Buried penis
- Occurs when the skin of the penile shaft has been lost because of severe inflammation, and the penis is trapped in the penopubic and scrotal area. These patients are often profoundly overweight, and many are diabetic
- Insert figure
Amyloidosis
- Rare disease of the urethra
- Should be considered in the evaluation of any patient with a urethral mass
- Patients present with hematuria, dysuria, or urethral obstruction
Male Urethral Diverticulum
- Pathogenesis
- Congenital vs. acquired
- Congenital: incomplete development of the urethra
- A congenital diverticulum in the prostatic urethra may be a large remnant of the müllerian duct associated with defects of diminished virilization.
- Injury of the urethra, which may cause an intraspongiosal hematoma
- Congenital: incomplete development of the urethra
- Congenital vs. acquired
- Diagnosis and Evaluation
- The tip of a urethral catheter tends to catch in the diverticular opening, necessitating the use of something to direct the catheter tip toward the true lumen.
- Management
- Other than necessitating caution during evaluation, these diverticula do not usually cause problems or require treatment unless they are very large.
- Large utricles can accumulate urine with voiding and then decompress after voiding. If they are large enough, the stasis of urine can be associated with recurrent urinary tract infection or difficult-to-manage “incontinence.”
- In many cases, endoscopic unroofing of the diverticulum remedies the voiding symptoms; although after unroofing, the patient commonly may note postvoid dribbling.
- Open repair essentially excises the redundancy of the urethra associated with the diverticulum.
- Other than necessitating caution during evaluation, these diverticula do not usually cause problems or require treatment unless they are very large.
Balanitis
- Balanitis, or inflammation of the glans, can occur as a result of poor hygiene, from failure to retract and clean under the foreskin.
- Balanoposthitis is a severe form of balanitis and occurs when the phimotic band is tight enough to retain inflammatory secretions, creating what amounts to a preputial cavity abscess.
Phimosis
- Inability to retract the foreskin
- Can result from repeated episodes of balanitis.
- Insert figure
Paraphimosis
- Painful swelling of the foreskin distal to a phimotic ring.
- Occurs if the foreskin remains retracted for a prolonged time.
- Management
- To reduce a paraphimosis, gentle steady pressure must be applied to the foreskin to decrease the swelling. When the swelling has been reduced, push against the glans with the thumbs, pulling on the foreskin with the fingers.
- An occasional patient presents with acute paraphimosis that has been present for many hours to days. In these cases, reduction may be impossible, and paraphimosis should be dealt with by emergency dorsal slit or circumcision.
Insert figure
Circumcision
- See CUA Circumcision Guideline Notes
- In adults, circumcision can be done with local anesthesia, by blocking the dorsal nerves at the base of the penis and circumferentially infiltrating the superficial layers of the penile base.
- In men and older boys, we favor a sleeve circumcision.
- Summary of steps:
- With the foreskin in its retracted position, a marking pen outlines an incision, leaving a small preputial cuff. This mark should go straight across the base of the frenulum. This incision is made and carried through the dartos fascia to the superficial lamina of the Buck fascia.
- The foreskin is reduced, and a second incision is marked, following the outlines of the coronal margin and the V of the frenulum on the ventral side.
- In some cases, the frenulum can be lengthened by closing the edges of the V in a longitudinal orientation for a short length (frenuloplasty). If frenuloplasty is done, the proximal incision does not need to follow the V of the retracted frenulum because the ventral skin is straight.
- We make the skin incision and fulgurate bleeding vessels with bipolar cautery as the incision is deepened and the skin edge is mobilized. In older boys and men, the vessels are more substantial and not easily sealed by compression, no matter how vigorous.
- After the sleeve of preputial skin has been removed, hemostasis is obtained, and the skin edges are reapproximated.
- Summary of steps:
- Complications should be uncommon.
- Most common immediate complication: hematoma
- Most patients develop some hyperesthesia of the glans, which resolves.
- Minimal separation may be amenable to healing by secondary intention.
- Some patients notice minor cosmetic imperfections that are functionally insignificant.
Failed hypospadias repair
- A hypospadias repair may fail because of an inadequate correction of chordee or an inadequate urethra, with a stricture, fistula, or diverticulum
Trauma to the genitalia
- See Lower Urinary Tract Trauma Chapter Notes
- Penetrating injuries to the penis can involve the urethra, the corporeal bodies, or both.
- With bullet injuries of the urethra, the velocity of the projectile must be considered. However, recent military actions have shown that high-speed projectiles can pass through superficial structures with relatively little cavitation effect and less propagation of energy to the adjacent tissues.
- Degloving injuries to the penis occur when the penis or scrotal skin is trapped and stripped from the deeper structures. Bleeding is usually not a problem. The tissues must be allowed to demarcate; acute reconstruction with grafts can be done.
- The damage caused by genital burns depends on how well the normal structures have been maintained after the acute injury. The unique vascular qualities of the penis allow careful repeated debridement as opposed to aggressive debridement.
- Radiation trauma to the penis occurs in two potential subsets: patients in whom radiation has been used therapeutically for a lesion on the penis and patients in whom radiation to the pelvis has caused chronic lymphedema.
- A patient with genital lymphedema can readily undergo reconstruction with either a STSG or, in select cases, the lateral margins and the posterior margins of the scrotum.
Urethrocutaneous fistula
- Pathogenesis
- Complication of urethral surgery
- Develop secondary to periurethral infection associated with inflammatory strictures or treatment of a urethral growth (condyloma or papillary tumor).
- Urethral carcinoma
- One must be cautious in a patient with urethral fistulae but without a history of chronic obstructive voiding symptoms. In many cases, fistula or periurethral abscess may be the hallmark symptom of urethral carcinoma.
- Management
- Varies according to the cause of the fistula and must be directed not only to the defect but also to the underlying process that led to its development.
Complex fistulae of the posterior urethra
- The interposition of omentum has been used for distraction defects and for complex fistulae. This approach allows safe mobilization of the rectum from the area of the distraction scar or from the fistula site.
- When radiation is added, the complexity of reconstruction is magnified. The effects of radiation must be allowed to settle; tissue interposition is the rule, and functional reconstruction is impossible in many cases. Some think that diversion, in the case of patients who have received radiation, is the safest and best option.
- Careful consideration of ultimate urinary and bowel function is integral to proper planning of surgery
Curvature of the penis
- "Chordee" means curvature.
- In curvature of the penis, there is relative asymmetry of one aspect of the erect penis. In some cases, this condition arises from diminished compliance of one aspect of the tunica albuginea or outright foreshortening of one aspect of the erectile bodies.
- Classified: congenital vs. acquired
- Congenital curvatures of the penis (ventral, lateral, or dorsal) are inevitably associated with the finding of a large erect penis.
- Acquired curvature is virtually always associated with trauma related to intercourse.
- Acquired Curvatures of the Penis That Are Not Peyronie Disease
- The lesion of a subclinical fracture of the penis is believed to be due to the disruption of the outer longitudinal layer of the tunica albuginea during the buckling trauma. The inner, circular layer is not disrupted and maintains the blood-tight continuity of the corpus spongiosum.
- Another possible scenario is that both layers of the tunica albuginea are disrupted, but the overlying Buck fascia maintains its integrity. Some patients notice a pop with intercourse and a period of pain with erections, followed by curvature of the penis—usually dorsal.
- In most cases, global cavernosal veno-occlusive dysfunction is not a complicating factor
Total penile reconstruction
- Forearm flaps are the most commonly employed method for total phallic construction and penile reconstruction.
- Dsadvantages to the use of a forearm flap for phallic construction:
- Obvious donor site deformity
- Possibility of the development of cold intolerance in the hand of the donor side
- Hair can be problematic when the forearm skin is hirsute
- Rigidity for intercourse in a patient with phallic construction is usually achieved by either an externally applied or a permanently implanted prosthesis.
- Prosthetic implantation is never undertaken until 1 year after phallic construction because protective sensibility must be demonstrated in the flap.
Questions
- What is the difference between a graft and flap?
- How long is the process of graft take? What are the 2 phases of graft take and how long does each take?
- What is the difference between a split-thickness and full-thickness graft? What has favourable vascular characteristics? Which is more likely to contract and be brittle when mature?
- Which grafts have successfully been used for primary urethral reconstruction?
- What is the treatment of lichen sclerosus?
- What is usually the cause of a prostatic urethral diverticulum?
- Which part of the urethra is most commonly affected in straddle injury? Distraction injury?
- List risk factors associated with urethral stricture disease
- A patient has undergone a urethroplasty and now has foot drop. Which nerve is most likely affected? Describe the sensory function of this nerve?
- While repairing a PFUI ,it is observed that the proximal urethral is significantly distracted in a rostral direction. Which maneuvers can be done obtain a tension-free anastomosis?
Answers
- What is the difference between a graft and flap?
- How long is the process of graft take? What are the 2 phases of graft take and how long does each take?
- What is the difference between a split-thickness and full-thickness graft? What has favourable vascular characteristics? Which is more likely to contract and be brittle when mature?
- Which grafts have successfully been used for primary urethral reconstruction?
- What is the treatment of lichen sclerosus?
- What is usually the cause of a prostatic urethral diverticulum?
- Which part of the urethra is most commonly affected in straddle injury? Distraction injury?
- List risk factors associated with urethral stricture disease
- A patient has undergone a urethroplasty and now has foot drop. Which nerve is most likely affected? Describe the sensory function of this nerve?
- Common peroneal nerve
- Posterolateral part of the leg and the knee joint
- While repairing a PFUI ,it is observed that the proximal urethral is significantly distracted in a rostral direction. Which maneuvers can be done obtain a tension-free anastomosis?
References
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 40