Anatomy: Groin and Inguinal
Jump to navigation
Jump to search
Groin[edit | edit source]
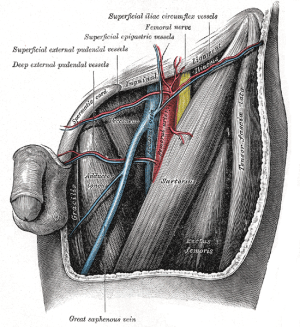
Vasculature[edit | edit source]
- Posterior to fascia lata
- Superficial vessels
- Supply the skin and subcutaneous tissue
- Branches of the femoral artery (3)
- Superficial circumflex iliac artery
- Smallest of the branches
- Pierces through the fascia lata
- Origin is usually lateral to the saphenous opening
- Travels superolaterally, in the direction of the anterior superior iliac spine
- Supplies
- Region of the skin over the lateral third of the inguinal ligament and the iliac crest
- Superficial fascia and superficial inguinal nodes along its course
- Anastomoses with branches of the deep circumflex iliac, superior gluteal, and lateral circumflex femoral artery
- Superficial epigastric artery
- Medial to the superficial circumflex iliac artery
- Following a more vertical course; ascends anterior to the inguinal ligament up to the region just below the umbilicus
- Typically originates from the anterior aspect of the femoral artery about 2–5 cm distal to the inguinal ligament, just inferior to the saphenofemoral venous junction
- Often originates from a trunk that is shared with the superficial circumflex iliac artery
- Supplies the skin, superficial fascia, and inguinal nodes in midinguinal area
- Branches anastomose with those of the contralateral artery and with the inferior epigastric artery
- Superficial external pudendal artery
- Medial origin on the femoral artery
- Rarely it may originate from the profunda femoris artery
- Medial route, coursing in the direction of the pubic symphysis where it traverses the spermatic cord in males and the round ligament in females
- Supplies cutaneous blood flow to the inferior abdomen, the penis, and the scrotum in males and the labia majora in females
- Anastomoses with branches of the internal pudendal artery
- Medial origin on the femoral artery
- Superficial circumflex iliac artery
- Anastomoses exist between the superficial and deep vessels
- Deep vessels
- Supplies the muscles and fascia
- Deep circumflex iliac
- Branches off of the lateral aspect of the external iliac artery
- Supplies the deep lateral groin
- Inferior epigastric
- Branch of the external iliac artery
- Origin just medial to that of the deep circumflex iliac artery
- Gives off two branches: the pubic and the external spermatic (or cremasteric)
- Forms the lateral border of the inguinal (Hesselbach’s) triangle
Inguinal Lymph Nodes[edit | edit source]
- Classified as superficial vs. deep inguinal nodes
- Fascia lata of the thigh separates the superficial and deep inguinal nodes
- Fascia lata is continuous with Scarpa fascia; transitions above the inguinal ligament
- Scarpa fascia is anterior to external oblique muscle
- Fascia lata is continuous with Scarpa fascia; transitions above the inguinal ligament
- Fascia lata of the thigh separates the superficial and deep inguinal nodes
- Superficial inguinal nodes
- Located deep to Camper’s fascia (also referred to as the superficial fascia) and superficial to the fascia lata (or deep fascia)
- Arranged parallel to the inguinal ligament
- Anatomic groups (5):
- Central nodes around the saphenofemoral junction
- Superomedial nodes around the superficial external pudendal and superficial epigastric veins
- Drain the prepuce of the penis and the scrotum
- Inferomedial nodes around the greater saphenous vein
- Superolateral nodes around the superficial circumflex vein
- Inferolateral nodes around the lateral femoral cutaneous and superficial circumflex veins
- 5–17 lymph nodes in this area
- A study using single-photon emission computed tomography (SPECT) scanning to assess lymphatic drainage patterns found sentinel lymph nodes to be present in the superior and central zones, which suggested that all modified inguinal lymph node dissections should include these two regions[1]
- Deep inguinal nodes
- Lies deep to the fascia lata
- Arranged parallel and primarily medial to the femoral vein in the femoral canal
- Tend to be in close association with the femoral vein
- 1-3 lymph nodes in this area
- Fewer in number, compared to superficial inguinal nodes
- Most cephalad of the deep inguinal nodes is the Node of Cloquet
- Node of Cloquet is
- Almost always present
- Located in the femoral canal between the femoral vein (medial to the femoral vein) and the lacunar ligament
- Lacunar ligament connects the inguinal ligament to the pectineal ligament
- Node of Cloquet is
- Receives drainage from
- Superficial group of lymph nodes
- Deep lymphatics that run with the femoral artery
- Glans of the penis and clitoris
- Drains into the pelvic nodes (namely, the external iliac, internal iliac, and obturator nodes
Femoral Triangle[edit | edit source]
Borders[edit | edit source]
- Roof: fascia lata (covers femoral sheath)
- Fascia lata is continuous with external oblique aponeurosis superiorly[2]
- Within the femoral sheath are the femoral artery and vein and the node of cloquet
- Fascia lata is continuous with external oblique aponeurosis superiorly[2]
- Floor: pectineus, ilacus, psoas major, adductor magnus muscles
- Superior: inguinal ligament (runs from anterior superior iliac spine to pubic tubercle)
- Inguinal ligament is the portion of the external oblique aponeurosis which extends between the anterior superior iliac spine and the pubic tubercle as a thick band, folded inward[3]
- Lateral: medial border of sartorius muscle
- Medial: lateral border of adductor longus muscle
- Apex: formed by the intersection of the medial border of the sartorius muscle and the lateral boarder of the adductor longus muscle
Contents[edit | edit source]
Lateral to medial: NAVEL
- Nerve
- Artery
- Vein
- Empty space
- Allows the veins and lymph vessels to distend to accommodate different levels of flow
- Lymph nodes (deep inguinal lymph nodes)
Nerves[edit | edit source]
- Femoral nerve
- Contains fibers originating from the L2–L4 spinal nerve roots
- Lies deep to the iliacus fascia
- Lateral to common femoral artery
- May at times be found between the artery and the vein
- Functions
- Motor: innervates the flexors of the hip and the extensors of the knee
- Pectineus, quadriceps femoris, and sartorius muscles
- Sensory: anterior thigh, anteromedial knee, medial leg, and medial foot
- Motor: innervates the flexors of the hip and the extensors of the knee
- Should be preserved during inguinal dissection.
- Some of the sensory branches, however, are commonly sacrificed in the regional node dissection.
Vasculature[edit | edit source]
- Posterior to fascia lata
- Common femoral artery
- Continuation of external iliac artery
- External iliac artery above inguinal ligament, common femoral artery below inguinal ligament
- Gives off a branch called deep (profunda) femoral artery and continues as superficial femoral artery[4]
- Blood supply to the skin of the inguinal region is from branches of the common femoral artery.
- Complete inguinal dissection necessitates ligation of these branches.
- Viability of the skin flaps raised during the dissection depends on anastomotic vessels in the superficial fatty layer of the Camper fascia
- A transverse skin incision least compromises blood supply to the skin.
- Complete inguinal dissection necessitates ligation of these branches.
- Medial to femoral nerve
- Just medial to the midpoint of the inguinal ligament in the inguinal crease region[5]
- Continuation of external iliac artery
- Common femoral vein
- Deep femoral vein and Great saphenous vein (also known as long saphenous vein) empty into the common femoral vein
- Great saphenous vein approaches common femoral vein medially
- Deep femoral vein approaches common femoral vein laterally
- Medial to common femoral artery
- Deep femoral vein and Great saphenous vein (also known as long saphenous vein) empty into the common femoral vein
Femoral Sheath[edit | edit source]
- A distal prolongation of extraperitoneal fascia that encloses the vascular compartment
- Femoral vessels and lymphatics are enclosed by the femoral sheath[6].
- Femoral nerve is located outside the femoral sheath
References[edit | edit source]
- Delman, Keith A., and Viraj A. Master. Malignancies of the Groin. Springer International Publishing, 2018.