Adrenals
Jump to navigation
Jump to search
Anatomic relationships[edit | edit source]
- Both adrenals are located at the level of the 11th or 12th ribs
- Right gland located more superiorly than left
- Recall that right kidney is located more superioly than left
- Right gland located more superiorly than left
- The adrenals are enclosed within the perirenal (Gerota) fascia and are completely surrounded by perirenal adipose tissue.
- Each gland is separated from the upper pole of the ipsilateral kidney by a thin layer of connective tissue
- The weight of each gland is ≈5g (range 2-6g)
- No variation between genders
- Recall that male kidneys are heavier than female
- No variation between genders
- Adrenal rests are found in proximity to the celiac axis and along the path of gonadal descent.
- Insert figure
Surgical landmarks[edit | edit source]
- Both adrenal glands are in close proximity to the crus of the diaphragm
Right gland[edit | edit source]
- Triangular
- Located nearly directly cranial to the upper pole of the right kidney
- Adjacent structures include the
- Underside of the liver anterolaterally
- Duodenum anteromedially
- Lateral margin of the inferior vena cava (IVC) medially
- Psoas muscle posteriorly
Left gland[edit | edit source]
- More crecenteric in shape
- Lateral surface is in contact with the medial aspect of the upper pole of the left kidney
- The adjacent structures include the
- Splenic vessels and body of the pancreas anteriorly
- Aorta medially
- Psoas muscle posteriorly
Vasculature[edit | edit source]
- Unique because the arterial and venous anatomy is highly variable
- In laparoscopic adrenalectomy, an adrenal artery is identified in only 1% of cases§
- Blood supply is redundant
Arterial Supply[edit | edit source]
- Sources (3):
- Superior adrenal artery, typically arises from the inferior phrenic artery, and rarely from the aorta, celiac axis, or intercostal arteries.
- Middle adrenal artery, typically arises from the lateral aspect of the aorta and rarely from the inferior phrenic artery or renal artery.
- Inferior adrenal artery typically arises from the superior aspect of the ipsilateral renal artery
- The superior arterial supply from the phrenic artery is constant; the middle and inferior arteries are variable
- Blood distribution within the adrenal gland
- Capsular arteries supply only the adrenal capsule and do not penetrate more deeply into the tissue.
- The medulla has two blood supplies
- Arterial blood from the medullary arterioles
- Medullary arterioles travel within the trabeculae of the adrenal gland to deliver blood to the medullary capillary sinusoids.
- Venous blood from the cortical sinusoid capillaries that have already supplied the adrenal cortex with arterial blood
- Fenestrated cortical sinusoidal capillaries supply the cortex and then drain into fenestrated medullary capillary sinusoids.
- This dual vascular supply is important for the medullary production of catecholamines
- As venous blood from the adrenal cortex reaches the medullary tissue, it contains a high concentration of glucocorticoids, and this situation plays a role in epinephrine synthesis
- Arterial blood from the medullary arterioles
Venous Drainage[edit | edit source]
- Both adrenal glands are drained by a single central vein that exits the adrenal anteromedially
- The right adrenal vein is short and enters the posterior aspect of the IVC.
- The left adrenal vein is longer and joins with the inferior phrenic vein and enters the cranial aspect of the left renal vein
Lymphatic Drainage[edit | edit source]
- Right: paracaval lymph nodes
- Left: para-aortic lymph nodes
Nerve Supply[edit | edit source]
- Sympathetic innervation of the adrenal gland causes release of catecholamines from the chromaffin cells of the medulla.
- Pre-ganglionic sympathetic nerve fibers from T11-L2 (lower thoracic and lumbar spinal cord) travel through the sympathetic chain to reach a nerve plexus at the adrenal capsule which then traverse the cortex to directly innervate the chromaffin cells of the medulla; there is no post-ganglionic innervation of the medulla
- Post-ganglionic fibers originating from the [parasymp vs. symp?] splanchnic ganglia provide innervation to the adrenal cortex
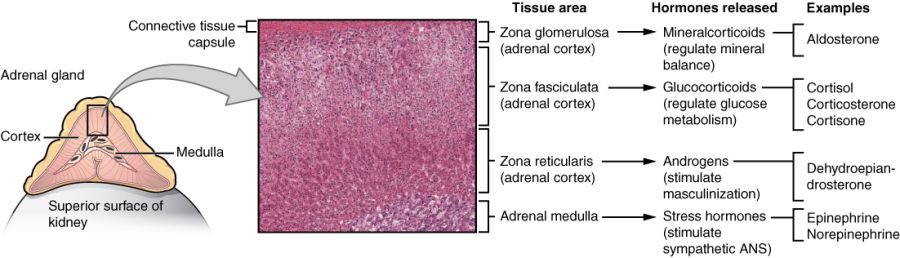
Histology of Adrenal Glands[edit | edit source]
- The gland is surrounded by a capsule
- Composed of 2 embryologically and functionally distinct components:
- Outer cortex
- Makes up ≈90% of the adrenal mass
- Endocrine component
- Derived from intermediate mesoderm
- Composed of 3 layers (from outer to inner):
- Zona Glomerulosa
- Comprises ≈15% of the cortex
- Produces aldosterone as a result of unique zonal expression of aldosterone synthase (CYP11B2)
- Zona Fasciculata
- Comprises ≈80% of the cortex
- Produces glucocorticoids as a result of zonal expression of 17α-hydroxylase, 21-hydroxylase, and 11β-hydroxylase enzymes
- Cortisol is the main glucocorticoid
- Zona Reticularis
- Comprises ≈5-7% of the cortex
- Produces the sex hormones as a result of zonal expression of 17α-hydroxylase and 17,20-lyase (3):
- Dehydroepiandrosterone (DHEA)
- Sulfated DHEA (DHEA-S)
- Androstenedione
- The sex hormones (DHEA, DHEA-S, and androstenedione) comprise the greatest portion of steroid hormone that is produced by the adrenals (>20 mg/day), but appear to be the least important for adult physiologic homeostasis
- Only 100-150 mcg/day of aldosterone and approximately 10-20 mg/day of cortisol are produced by the glands.
- Zona Glomerulosa
- Inner medulla
- Neurocrine component
- Derived from neural crest cells that later give rise to chromaffin cells
- Chromaffin cells of the medulla secrete the catecholamines (3):
- Epinephrine (80%)
- Norepinephrine (19%)
- Dopamine (1%)
- These catecholamines are produced from the amino acid tyrosine
- The adrenal gland is the primary source of systemic epinephrine
- Despite the presence of similar chromaffin cells elsewhere in the sympathetic nervous system, the enzyme phenylethanolamine-N-methyltransferase (PNMT), which catalyzes the conversion of norepinephrine to epinephrine, is relatively unique to the adrenal medulla (the brain and organ of Zuckerkandl also express this enzyme)
- Outer cortex
Radiology[edit | edit source]
- US
- More commonly used for differentiating between solid and cystic masses of the adrenal gland.
- The retroperitoneal adipose tissue can make it difficult to differentiate normal adrenal tissue from the surrounding structures
- More commonly used for differentiating between solid and cystic masses of the adrenal gland.
- CT
- Most widely used imaging modality for imaging the adrenal glands
- Normal adrenal tissue (including adenoma) has a density of ≤ 10 Hounsfield units (HU) on non-contrast scan
- MRI
- Contrast resolution with T1-weighted and T2-weighted images is superior to that of CT
Questions[edit | edit source]
- What is the typical arterial blood supply to the adrenal glands?
- Where do the adrenal veins drain to?
- What are the 3 zones of the adrenal cortex and what do the secrete?
- Describe the autonomic innervation of the adrenal medulla
- Which enzyme catalyzes the conversion of norepinephrine to epinephrine?
- What are the catecholamines produced by the medulla? From which amino acid are they made?
Answers[edit | edit source]
- What is the typical arterial blood supply to the adrenal glands?
- Superior adrenal artery arising from the inferior phrenic artery
- Middle adrenal artery arising from the aorta
- Inferior adrenal artery arising from the adrenal artery
- Where do the adrenal veins drain to?
- Right adrenal: IVC
- Left adrenal: renal vein
- What are the 3 zones of the adrenal cortex and what do the secrete?
- Glomerulosa: aldosterone
- Fasiculata: cortisol
- Reticularis: sex hormons
- Describe the autonomic innervation of the adrenal medulla
- Preganglionic sympathetic nerve fibers act directly on the medulla, there are no postganglionic fibers
- Which enzyme catalyzes the conversion of norepinephrine to epinephrine?
- PNMT (phenylethanolamine-N-methyltransferase)
- What are the catecholamines produced by the medulla? From which amino acid are they made?
- Dopamine, noepinephrine, epinephrine
- Tyrosine
References[edit | edit source]
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 64